Understanding Tongue Tie: More Than Meets the Eye On my intake form I often receive a comment such as:"My midwife said my baby has a slight tongue tie” or “the pediatrician said there is small tongue tie but it nothing to worry about.” Let's dive into this topic and explore why tongue tie is more than just a visual examination of the tongue and why it requires proper attention. What do we even mean when we say Tongue Tie? This is where the tissue connecting the tongue to the floor of the mouth (lingual frenulum) is shorter or tighter than usual. This can restrict the movement of the tongue, potentially causing difficulties with breastfeeding and other oral functions. It can restrict motion in more than one direction - not just out. Some babies may have a tongue tie where the frenulum restricts the tongue's movement significantly and it is very obvious visually. Others may have a tongue tie where the restriction is less pronounced. This is likely why people say “slight tongue tie.” When it comes to breastfeeding we need to do a functional assessment. While a visual examination of the tongue can provide some initial insights, it's not the sole determining factor. The impact of tongue tie on breastfeeding can vary from baby to baby, and it's essential to consider other factors such as latch, milk transfer, and maternal comfort. If you suspect that your baby's tongue tie is affecting breastfeeding, it's crucial to seek guidance from a lactation consultant experienced in assessing and treating tongue tie. They will evaluate your baby's feeding patterns, observe the latch, and consider other factors to determine the best course of action. The goal of an assessment is to identify concerns that are presenting and/or being created. From there a plan to improve those aspects of breastfeeding and ensure both mom and baby are comfortable and thriving can be created. This plan can range from actions to improve intake and heal any trauma the breast/nipple has sustained and treatment. Not doing so results in babies who are not growing as expected, low milk supply and maternal pain amongst other concerns. If you've been told that your baby is "just a little tongue tied," it means that there may be some degree of restriction in tongue movement, but it may not be severe enough to cause significant breastfeeding challenges or it may not be presenting concerns YET. However, it's always worth seeking professional guidance to ensure optimal breastfeeding success. This also helps to understand why I say no concerns YET. Breastfeeding changes so much in the early days & weeks that it is not uncommon to see a tongue tie that was not causing any issues at 2 days does cause issues at 2 weeks. Tongue ties undoubtably have an impact on breastfeeding and it is important to seek proper evaluation and support. By doing so you can be empowered to navigate breastfeeding with confidence. The Beauty and Challenges of Breastfeeding: |
| Really, I was thinking to myself, these people are INSANE. As a fellow insane person, I opened my mind and listened to what people had to say. I heard them out. I decided to change some things in my practice and assessments. I grew myself. I pushed myself to really learn more. Truth was, people were making history at that time. We were in it. It was a time of ah-ha moments all over the place. No one had all the answers about tongue tie and their related issues, but many had theories. |
I dove in. I recruited other professionals as supports. We networked. We shared experiences. We re-evaluated. We want the best for families.
My job as an IBCLC is not the same as those other supports and professionals but I want to share some of my learnings and reflections. I know tongue ties cause a lot of issues. I will not deny that, but I will say that just “getting it snipped” or getting into a dentist for a laser revision isn’t a guarantee things are going to be resolved.
A really key piece I have acknowledged is how much better babies that are at an appropriate weight recover and catch on to breastfeeding post-revision compared to babies that are underweight or slow gaining, maybe gaining weight a little faster than what is called a slow gainer and who maybe is not getting much concern from anyone but still not growing on “their curve”. Doing a revision on these babies is something I really hesitate to do now and I won’t make a recommendation for revision until resolution has occurred in the weight department. This to me a really good reason to be working with an IBCLC before hand.
Another really important part to working with an IBCLC is to assessing milk supply. Babies respond to flow and without that flow, they just won’t want to try and improve anything. Add in a tongue tie and they just don’t care to breastfeed nicely or at all. If supply is low, again even with a revision, they just are not happy breastfeeders. Both this scenario and the above one make people say “the tongue tie wasn’t the issue” and sometimes add in that “they did the procedure for nothing”. Being able to get moms working on supply, which in turn can help the weight gain issue, if it exists, helps ensure that once they get those two factors sorted out, they are ready for revision and have a good foundation to make the revision successful. The pieces fall into place nicely and almost predictably. It also helps me be able to tell a mom a timeline for “when will this all be better”. I can help them set up a plan so they can see a means to an end, rather than “just keep trying, it will click soon”.
There is also maternal pain that is often a concern and should be addressed INDEPENDENTLY of a revision. Sometimes tongue ties cause pain, damage & trauma to mothers breasts and can be resolved with a revision, but ideally more should be done to address this instead of just waiting for things to get better. When we deal with the breast/nipple independently, it makes the revision seem significantly more effective.
Babies can have other factors/stresses affecting and influencing breastfeeding that are often identified by IBCLC’s or professionals who assess physical factors, like Chiropractors or Osteopaths. I also find when we resolve these issues first, or at least start working on them, that things get back on track faster post-revision.
Sometimes I am not consulted until after a procedure for a tongue tie has been performed. When I get called after, I can most certainly still help and we can get past these remaining pieces, it just is in reverse. What I find though, is it is all a lot more stressful for moms and families because they also have a cranky baby and after care exercises to get in, as well as possible pumping & supplementing, and perhaps appointments with the other professionals we work with. I personally think It is better when I can set up a plan in steps with one focus at a time. Once supply and weight is up, it is one less stress, so the family can handle the stress of the aftercare and extra needs of the baby.
I am also aware that some parents would rather not go through a revision at all and this is where my “Before Tongue Tie” experience and knowledge comes in. I say to the parents and myself, “what would we have done BTT?” Are there strategies that would be useful and address the concerns? Sometimes there are solutions that the parents are 100% ok with and will get the baby fed and minimize concerns. Sometimes all of those are tried and the revision conversation might have to happen again. This is where knowing the risks to the situation and knowing what else to watch for is important.
Tongue ties are a topic that people get really excited about from many different perspectives and I don't see that changing for awhile, but I wanted to raise the thought that we are in a place of breastfeeding right now that in the years to come will be a historical recollection. It might be known as something more eloquent than BTT but until then we can recall what it was like BTT.
Canadian Pediatric Society no longer recommends this practice from the late 1800's (it is now 2017)
9/6/2017
Neonatal ophthalmia (NO) is a relatively common infant illness & is defined as conjunctivitis occurring within the first four weeks of life. This term originated from cases caused by N gonorrhoea, but the term now currently refers to any conjunctivitis in this age group.
In most instances, neonatal ophthalmia is a mild illness and can easily be treated case by case once infectious conjunctivitis is determined & distinguished from eye discharge secondary to blocked tear ducts and from conjunctivitis due to exposure to some kind of irritants or chemicals. The exception to this is ophthalmia due to infection with N gonorrhoea. Those cases are quite dangerous for infants.
A lot has changed in Canada since then and the Canadian Pediatric Society is no longer recommending routine prophylaxis for neonatal ophthalmia. The primary reason is that N. gonorrhoea strains isolated in Canada are showing considerable resistance to the treatments routinely used and there are no recent studies of the efficacy of ophthalmia prophylaxis with these treatments.
You can see the position statement, complete recommendations from the CPS and the history of NO, risk factors & legal considerations depending on where in Canada you live on the Canadian Paediatric Society website.
I want to be *explicitly clear* that this is NOT about individuals. This is not about the idea or execution of such events. This is not about women supporting or not supporting women. This is not about businesses who chose to plan events. This is not about businesses who participate in events. This is fully about the sponsorship by the companies covered by the WHO Code. (and I promise you they all know about the WHO Code and how that impacts their relationships).
So, what is the WHO Code?
The purpose of the Code is to protect breastfeeding, to protect all mothers and babies, regardless of their desired feeding methods, and to prevent aggressive marketing practices that often interfere with mothers meeting their own breastfeeding goals. Infant formula, feeding bottles, and artificial nipples are the main products that fall within the scope of the Code. Breast pumps are not under the scope of the Code BUT some pump companies violate the code because they market bottles and artificial nipples. Again, the Code only applies to the marketing of these items–it does not affect whether they are sold or used. Confusing, right?
Confused? Of course you are!
Then we have to consider who are the "kid" companies and who are the "parents"? Companies who are owned by Code violators are considered the same as their parent company. You really have to dig deep to find out a lot of this info, but if you start goggling different brands of formula, medications, infant supplies, etc you start to see that there are a lot of kid companies and just a few parents. The parent companies, of course, want to keep their smaller companies WHO Code violating record clean so that health care workers who have to adhere to the WHO Code can still have relationships with these companies, while the parent company gains benefits. They can also give items and samples not covered by the WHO Code and maintain compliance. But in the end, they are still violators.
As an IBCLC, I need to educate people about the WHO Code and marketing. What I am encouraging people to do, all across Canada, is to just keep their eyes open a little bit to who is hosting events, who is sponsoring events, what is that relationship like, who is providing the educational piece & decide if the information being given is evidence based and helping mothers meet their breastfeeding goals or if the information might be slanted. You will see a large variety of how these events take place and some will be absolutely ok and some are going to have questionable practices.
This is not about you and it is not about me.
I want this to be heard by everyone because if the doula/nurse/doctor/pharmacist or IBCLC, asked to participate this time walked away, the companies will just go to find another one. This also applies to educational events for professionals so not only do we look down, we have to look up. I want parents to hear this so if they go to an event they can also see who is providing the funding for the event and the information.
Eyes open!
I am here again suggesting you keep again breastfeeding old faithful on the shelf! At bare minimum before taking fenugreek to help an unsteady to low supply, keep that bottle of fenugreek sealed until some further investigation as to why you might need something to boost supply is started.
I think “breastfeeding issues” are sometimes breastfeeding issues but I also think that often time struggling with breastfeeding is just a symptom of something else. Paying attention to your supply as an indiction of something else, might actually help you understand more about your body and its personal needs.
This is not to say there are not good herbal options for supply, because there are. It is matter of knowing what is happening with your supply and your body, your own unique challenges and having a health history taken or worked up, so that the right herbal for each individual can be chosen/suggested. It might just be fenugreek for you. But, there is a good chance there is something better.
I will also add that many mothers experience upset stomach, gassiness, loose stools, diarrhea, dehydration, low blood sugar & unpleasant body odour when taking fenugreek. Baby may also show similar symptoms.
If you have never considered becoming a Surrogate Mother, and are not in a position to need the help of surrogacy to become a parent, you may be wondering why anyone would want to become a surrogate.
We find there are four main reasons the people we work with want to give the amazing gift of parenthood to others!
“It” can be anything. Most of the Surrogate Mothers I have talked to over my years of involvement in surrogacy choose to become Surrogate Mothers because they want to spread the good and love in the world. These amazing women just want to be a source of light in the lives of others. I cannot think of a more beautiful way to perpetuate positivity.
Women choose to become Surrogate Mothers because they believe everyone deserves a chance to be a parent.
I have found many people who are called to surrogacy are warriors for social justice. They see how difficult it is for those seeking the assistance of a Surrogate Mother to become parents. Their hearts break for the single Intended Parents, gay couples that are desperate to become fathers, older couples who have yet to experience the joy of parenthood, cancer survivors, and others who have been struggling to adopt or have children on their own. Egg Donors and Surrogate Mothers are the balance that can tip the scales of inequality for Intended Parents.
Having experienced and overcome infertility, people become Surrogate Mothers to give the gift they have been given.
Some of the Surrogate Mothers I have worked with or spoken to have decided to pursue surrogacy because they required the assistance of an Egg Donor or Sperm Donor to become a parent but were able to carry their baby. Others fought long, and hard battles with Infertility and by chance became pregnant. Their empathy and compassion for others is strong, having experienced infertility themselves.
A woman may choose to become a Surrogate because she loves motherhood and being pregnant.
Some people abhor being pregnant and view it as a necessary means to an end. Others have never felt more beautiful than when they are with child. Combine that with the joys of being a parent, even when it's the most thankless, draining job in the world, being a parent is incredibly rewarding. For some, choosing to become a surrogate is as simple as wanting to enjoy pregnancy but being finished having children of their own and wanting to help others experience parenthood, too!
Surrogacy in Canada is altruistic. This means that everyone who chooses to be a Surrogate Mother in Canada does so out of the goodness of their heart. One cannot be compensated for their surrogacy journey (although all related expenses will be reimbursed). Surrogate Mothers are truly giving a gift that cannot be repaid. I am constantly in awe of the Egg Donors and Surrogate Mothers I meet. Their selflessness becomes a miracle for others. They truly give the gift of life.
A surrogacy consultant with Proud Fertility, our guest blogger Nathan Chan has made it his life work to help people fulfill their family dreams.
Watch the video below to hear Candice's story with surrogacy.
Mary Poppins even brought her own lights. Lights are important, but again, I am not worried about the lighting at the hospital or your home. Even if you want dim lights, the doctors and midwives have flashlights - yes, they do! Speaking of lights, some people like to have some flameless candles to create a nice ambience. I do have some in my doula bag, but as an FYI, they are a few dollars at the $1 Store.

Mary Poppins has a mirror in her bag and I sure could use a mirror in my bag. It would be perfect for that moment the baby is crowning and a mother wants to look. Hold on, wait, that hasn’t happened. I have yet to have a mother giving birth who wants to see….
Now, of course, I know some moms would want to but in my experience it is not super common. Again, if that is something you think you might want to try in your birth, lets chat about it and make a plan about who should bring the mirror, just like the plant.
That tape measure Mary Poppins has in her bag is amazing and I would love one! I mean imagine being able to measure up people I am going to work intimately with and be told all about their personality. Wow, what a benefit that would be to me and to my clients. Wait, hold on. I do often have a tape measure in my doula bag…with my knitting. Yes, I pack knitting into my doula bag. What? Why on earth would I have knitting? We can talk about that later in another blog post.
Back to this tape measure idea. I don't have a tape measure that will tell me easily what your personality is, but I do however have a tool that will help me discover more about your personality and help me connect with you to make our work together easier and a little more flawless. The “Your Birth Experience” (YBE) program allows me to connect with you, identify your needs and then equip you with the resources necessary to achieve your goals. This leave mothers and their families empowered to envision their ideal birth, prepare for that birth and ultimately achieve the birth experience they desire. That’s pretty close to the magical tape measure, right? It is close enough for me.
So far you now know my doula bag has a few tea lights, running shoes, knitting and a tape measure. That tape measure isn't the good personality one - that comes from our prenatal meetings. That is all I have in my doula bag? Don't I have a rebozo, massage balls, TENS machines, birth balls? Nope. I do have some gum, some cash for parking, some hair ties and some snacks. Why some simple? Largely, infection control. For real, I don't want to disinfect birth balls and I surely don't want to clients sharing “dirty” ones. I don't want to have to wash beautiful fabrics in harsh chemicals made for industrial disinfection standards. I sure can do some neat stuff with a hospital sheet that I can get at the hospital and then leave at the hospital to have cleaned properly, just like the birth balls. Massage balls and TENS machines…what can be bad there? Nothing is really bad, but I prefer to not place an object between my clients and I. I find a better connection with direct contact and that increases endorphins which are great for labour. Again, if clients know they want to try a TENS machine or like the porcupine balls, I can help them use ones that they likely already own.
What I do have that cannot be packed into a bag is my years of experience and my confidence. Relief comes to my clients simply by my being present, much of the time. Clients know they can count on me to be present for them. I am a familiar face they know already and our relationship is solely focused on me helping them have a positive experience. They are presented with a bendy straw in a cup of water to juice, before they even knew they were thirsty. I am leading them to the washroom to pee and get that bladder out of the way of babies path because they didn’t realize they needed to pee. I am lightly touching and stroking their feet to remind them to relax their WHOLE body. I am that voice in their ear telling them that they can and are “doing it” when they feel like you are not being strong.
The thing is, people don't give birth every day, (truth be told, I don't attend birth everyday), but I do support women giving birth more often than the average person will give birth. I have been alongside many others before. Each experience is different and no path looks the same, but they are similar enough that I can follow the flow and go alongside and help women through it. They can say things like “Is this normal?” or “what else can I do?” or “what did that nurse/doctor/midwife mean?”. I will reassure them things are normal and they are doing great, I will make suggestions about what else they might want to do, or reassure them what they are doing is perfect & I will help them understand what the care providers are doing or saying. I can help the partner and encourage them just as much (maybe more, maybe less) as I do a labouring woman.
My doula bag started out full of items, and honestly, I could have taken a small suitcase on wheels to births when I first started because I felt like I needed to bring it all. I how know that to "bring it all", we need to do more work in the time before labour, and when I “bring it all” now, I am bringing our conversations, unique goals, unique desires, unique choices and my confidence, my experience and can be “tricky” just like Mary Poppins. I am confident I can pull stuff out of thin air that will help me meet your needs without carrying a lot of baggage.
If you would like to explore the idea of having a doula support you during your birth, I would love to hear from you.
Here are 15 things you might not already know about vernix:
- The formal name is Vernix Caseous. Vernix means varnish and caseous means cheese-like.
- It is a naturally occurring biofilm made in the last trimester of pregnancy.
- The first mention of vernix was in the Dunglison dictionary of Medical Sciences in 1846. 1846. Can you believe that? And here we think we are on to something new these days.
- Vernix is unique to humans.
- At the time of birth, vernix might cover the entire body of an infant or it might only be found in the body folds of the baby.
- Vernix might take on a more yellow, green or brown colour instead of the typical white colour. These colours might reflect intrauterine problems or fetal distress.
- Vernix is 80% water and 20% lipids and proteins.
- Vernix, combined with amniotic fluid, is swallowed by the fetus in utero & has a positive impact on gut development.
- Vernix acts like lubricate of the infant during delivery.
- Vernix is antimicrobial. It is an antimicrobial agent that protects against the bacteria filled environment of the mothers vaginal area. It provides an acidic environment on the skin which is believed to inhibit the growth of problematic bacteria.
- Vernix acts an insulator post delivery as the baby transitions into the outside world and helps babies regulate temperature. (This can continue for up to 5 days if left on the infant.)
- Vernix is a great moisturizer and has amazing wound healing properties (studies are being done on burn injuries).
- Vernix is believed to have antioxidant properties, which helps aids against the stressors of birth.
- Vernix blocks out meconium contamination of amniotic fluid.
- The National Association of Neonatal Nursing (NANN) and the Association of Women's Health Obstetrical and Neonatal Nursing (AWHONN) released a consensus statement that states “removal of all vernix is not necessary for hygienic reasons” and “vernix may provide antibacterial promotion and wound healing”. The World Health Organization (WHO) also recommends leaving vernix intact on the skin surface after birth.
I think we can agree vernix is pretty amazing.
The term lactation consultant or LC has become the known, accepted title for a professionals with expert knowledge in breastfeeding. They may work with moms and babies to address breastfeeding issues and concerns. They may also teach classes, assist with establishing breastfeeding one on one, and promote and protect breastfeeding through policy, procedure within health care and government.
Origin of the term “Lactation Consultant
The accepted term for “IBCLC” or International Board Certified Lactation Consultant in many geographical areas is "LC" or Lactation Consultant because, as you can see, that term is a mouthful.
“LC” is not trademarked and does not hold the professional standard like “IBCLC” does, so one will occasionally find a practicing LC who is not an IBCLC. Consumers (mothers and families) and other professionals (doulas and doctors) need to be aware of this.
As well, not all those who work as “lactation consultants” in health centres or breastfeeding support centres are IBCLCs. Some employers encourage employees to pursue the credential but don’t mandate it for employment. Many times, nurses with some basic breastfeeding education fill these jobs.
Why is this IBC part so important?
The International Board of Lactation Consultant Examiners (IBCLE) awards the title of International Board Certified Lactation Consultant to only the candidates who meet the comprehensive pathway requirements and pass an international exam. This allows IBLCE to establish the highest standards in lactation and breastfeeding care worldwide and to certify only the individuals who meet these standards.
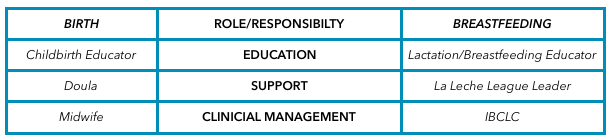 Breastfeeding education, support, clinical management
Breastfeeding education, support, clinical management Breastfeeding alphabet soup
I’d like to explain some of the breastfeeding alphabet soup by using the birthing support alphabet soup, as people seem to relate to that.
All the roles are important, but they provide their own distinct scope, responsibilities, and abilities. They can all work together to provide comprehensive support.
Primary roles of the individual bodies
As you can see, I’ve broken this down into three primary roles.
1. Education
2. Support
3. Clinical management
Education
Educators teach you about the normal and expected processes of childbirth and breastfeeding. They typically call themselves childbirth educators and lactation educators.
They teach the normal process of birth and what you can expect when having a baby, as well as encourage and promote breastfeeding.
This information helps you make decisions, helps you know if you are on track, gives you references for getting the birth and breastfeeding relationships you want, and helps answer your questions.
Educators typically teach community classes in group settings.
Support
Support people are typically those who have additional training in supporting mother, baby, and family during crucial times: birth and breastfeeding.
They’re typically doulas and La Leche League (LLL) leaders. Doulas are usually paid professionals, and LLL is a mother-to-mother peer support group. These roles offer the encouragement and motivation you need to get through the processes of birth and breastfeeding.
They are well versed in normal and expected outcomes. They know to watch for red flags to ensure they can guide you further if you have come outside the normal, expected process. Their job is to provide physical and emotional support, encouraging you to ask questions of your caregivers to make sure you’re well informed about what occurs. They have resources and guidelines to reassure you that you’re indeed in the realm of normal, and if things deviate from normal, they can point you in the direction of more resources.
Clinical management
Lastly, we have the clinical management professionals.
These are the folks responsible for the clinical and medical bits of the scenario. They look at the facts and figures, big picture, and red flags to rule in or out the things that are not in the normal and expected category and then make management plans from there. They have the clinical experience of things that fall outside normal and how to manage them.
Working together
All of these people have a place in the realm of support and caregiving; what’s important is they know their role and responsibility and respect the others’. Where it becomes problematic is when the client receives something different from what she expected to receive. Sometimes, this occurs because the roles of each provider isn’t clear to her, and she might conclude that one person isn’t performing a role properly. Let’s look at how this might apply to IBCLCs specifically.
In our example, a mother assumes that a breastfeeding educator* is an IBCLC. She notices that despite consulting with the helper, her breastfeeding issue remains unresolved. She decides to seek more help through a La Leche League leader, who determines that the issue is outside her scope and recommends an IBCLC. The mother insists that she already saw an IBCLC, but received no help.
*this person could also be staff at a breastfeeding clinic or nurse who comes to her home
This example is typical, and it hurts all support people. The educator gets a bad rep because she didn’t help. The LLL leader is helpless because the needs were outside her scope. The IBCLC profession gets a bad rep because the client misunderstood the different roles and expectations.
Clients need to know clearly what their expectations are and who can best meet those expectations based on role, scope, and experience. I want to be asked and welcome being asked these questions! I want you to go and look at the IBLCE website to see what IBCLC's are all about and verify I am indeed and IBCLC and see what scope and standards are laid in place for my profession. I welcome the same questions about being a doula! I would love to see a blog about midwives and how they are different from doulas and childbirth educators (wink, wink, nudge, nudge midwives).
All breastfeeding and lactation professionals have a responsibility to work together to ensure mothers have accurate information, so they can receive the support and encouragement they need as efficiently and as quickly as possible.
It is a based on one of those HOT parenting topics; SLEEP!
This is the perfect handout for you! Hope you find this resource helpful and reassuring.
Simple Ways to Calm a Crying Baby
... and Have a More Peaceful Night’s Sleep

It is true that all over the place, in so many places new and expecting parents are visiting, there are posters and flyers and brochures and people encouraging breastfeeding and exclusive breast-feeding. This recommendation is world wide and comes from the World Health Organization. While I agree with all the benefits of breastfeeding, as most people would, it is NOT enough to just give benefits. In fact, it is dangerous to encourage and promote breastfeeding & yet not be able to follow through with the support needed. Breastfeeding is significantly more complex than the two-dimensional vision posters make it out to be. Most women are certainly not relating to the mothers on the photos of the breastfeeding books. You know, the mothers who have perfect skin, no bags under their eyes, pristine hair and makeup looking like they have zero cares in the world…beyond oxytocin highs.There needs to be support for the mothers that can breastfeed "easily" so they succeed. We also must meet the needs of and support the mothers in which breastfeeding is not going to work "easily" or perhaps not at all….and all the unique, complex cases in between this. Blanket statements are harmful, on all sides.
Supports for new families are getting less and less available and the resources we do have are not always adequately trained and skilled to handle the cases they have presented to them. For every mother who feels judged because she could breastfeed, but doesn't want to, there is another mother who is feeling judged because she wanted to breastfeed, but did not meet her goal. There are mothers who celebrate being told their babies need to be supplemented and welcome supplementation. There are mothers who are devastated when they are given the same news. We need to learn how to support all kinds of mothers and all kinds of scenarios. We have to be prepared for that to take more than 5 minutes in the doctors office.
Let's look at one way this all gets blurry. There are the mothers with babies who are not sleeping well but the mother has been reassured that this is just how breastfeed babies are. I don't believe that to always be the case…sometimes babies are not sleeping because they are hungry…breastfeeding is not working in that case, not for anyone. Mothers and babies need to sleep. Feeding endlessly for days and weeks is not healthy for anyone. The issue then becomes "exhaustion due to breast-feeding" weeks later, when breast-feeding issues could have been addressed, resulting in more sleep. Beyond that, families need support people to come in and do practical stuff, like care for a baby so mothers can nap, feed themselves, go for a walk. That doesn't mean breast-feeding needs to be discontinued, it just has to be understood and managed. Other examples would be a woman in so much pain from breastfeeding. Who wants to torture themselves 10 times a day. That is a breakdown waiting to happen. Again, lets get to the source as soon as we can. Get to the resolution so the mother can be pain free. There are so many options for that.
We know about postpartum blues and depression and how common it is. We also know that for many women it is so bad they are taking their own lives. It is horribly, horribly sad and devastating. I don't believe it is about mothers breastfeeding or not. I believe it is about support, or lack there of, about misunderstanding babies and mothers, about isolation and healthcare systems that seem to be set up for failure and not success, it is about misunderstanding what the Baby Friendly Initiative is and what it was intended to do and how it is supposed to work.
We can do better. We need to do better. Lives matter and are being lost.
It is said that less than 6% of mothers use a doula for their births. That could be because many people have no idea what a doula is. It can also be that there are misconceptions of what a doula is and what a doula does. Doulas are certainly not new and there are many stories of how doulas originated.
A modern day doula is known as a non-medical support person for pregnancy, birth and postpartum (the time after the baby is born). A doula can be a source of encouragement, empowerment or simply a coach to the birthing person and their partner. Modern day doulas work professionally, confidently and comfortably alongside medical care providers such as doctors, midwives and nurses.
A doula is a constant in the process. They meet with people during pregnancy and remain into the postpartum period. In a system where care providers rotate and work in shifts, there is often change in who is looking after a birthing woman, as labour can take more than one shift, maybe two (sorry, maybe more). Feeling safe and secure can be difficult around strangers and often the time is not there to develop relationships with the care providers. A doula can help keep feelings of safety and security by being a previously known relationship and remaining as a constant. With that in place, a doula can help bridge relationships with the changing staff to make the transition easier on the labouring woman.
2. You are worried a doula will not allow you to make your own decisions about your birth.
Now that we know a bit more about what a doula does, one might wonder if they will tell people what to do for their births…the good news is doulas should be unbiased in their support of individuals. A doula might have particular views on how she would have a baby, but that should not be projected onto a family. I am supportive of all kinds of births. I want people to aware of what their choices are. Did you know people have choices in pregnancy, labour and birth?

A caesarean section is no less of a birth than any other birth. A doula can help prepare expecting families for the upcoming birth. They can help you formulate questions you might have for your care provider. They can help you prepare for what the procedures & processes of the day may be. They can even help you plan a birth plan for the day. Even with a scheduled caesarean birth there are still options and a birth plan is an ideal way to communicate those choices. While waiting for the birth a doula can help ease parents mind and help them prepare emotionally for the birth as they would during a labour setting. There are uncomfortable moments preparing for a caesarean, like an IV or epidural, and doulas help support parents through those moments. Inside the operating room, a doula can provide details that parents would like to know about. The doctors and nurses are busy with taking care of mother and baby. The partner is awaiting the baby and may feel uneasy in the hospital setting. Doulas are there to support partners as well. If the baby has to go to another area of the hospital, the partner can follow along with baby, and the doula will remain with the mother. This is reassuring to both new parents. Mothers do not need to be alone at all during a caesarean. Doulas also help in the postpartum period such as breastfeeding and making sure the mothers is comfortable and doing as well as she can be after the birth.
4. You have a midwife
As I said above, modern day doulas work professionally, confidently and comfortably alongside medical care providers. Midwives and doulas are a complement to each other. Midwives are experts in pregnancy and birth and the most compassionate people who provide amazing support to families. However, they have the primary responsibility to be clinicians which is quite different from a doula. They have a lot of things to set up, monitor, chart, etc and often have to take off the unbiased support hat they wear and move into more of a decision making role or give an opinion as to what they feel is best and safest for mother and baby. They might even have to be taking care of more than one family at a time. If things are calmer and quiet, sometimes midwives leave to go and rest/sleep while a woman is labouring, so she can be rested and in her best mind and ability for the birth. Having a doula there means mothers is continuing to receive emotional and physically comfort.
5. You don’t need one
You are giving birth to the baby, and that is one fact we cannot change, but the experience of birth often includes another person - the partner. Sometimes the partner is who needs that constant support and encouragement. I have been invited back to be a repeat doula for families I have served previously, not because the mother feels she needs a doula, but because the partner did not want to go through the process without a doula. Sometimes as a doula, providing support and encouragement to the partner, means the partner is who shines in the mothers eyes as her primary support person. That is wonderful! I love when that happens as birth should belong to that couple.
And, maybe, truly, neither person needs a doula. I do not believe doulas are needed at births…you know, those babies are coming out at some point regardless of who is at the birth. Doulas are not a must have, doulas are an added extra. Doulas are a must have for some people, but not all people, and I support that decision.
If you would like more info on the doula services I provide, I have more information readily available for you.
Kim Smith
IBCLC,
Chatting about a variety of birth and breastfeeding topics.
Categories
All
Breastfeeding
Breastmilk Donation
Childbirth
Doula
Essential Oils
IBCLC
Lactation
Low Supply
Pain
Postpartum
Sleep
Thrush
Tongue Tie
Vasospasms
Weight Gain
Archives
September 2023
May 2022
September 2021
July 2021
February 2020
January 2020
April 2019
February 2019
January 2019
December 2018
October 2018
August 2018
June 2018
April 2018
September 2017
August 2017
April 2017
February 2017
January 2017
September 2016
August 2016
July 2016
June 2016
April 2016
March 2016
February 2016
December 2015
November 2015
October 2015
September 2015
August 2015
July 2015
May 2015
March 2015
February 2015
January 2015
November 2014
May 2014
April 2014
March 2014


















 RSS Feed
RSS Feed
