The Beauty and Challenges of Breastfeeding: |
| Really, I was thinking to myself, these people are INSANE. As a fellow insane person, I opened my mind and listened to what people had to say. I heard them out. I decided to change some things in my practice and assessments. I grew myself. I pushed myself to really learn more. Truth was, people were making history at that time. We were in it. It was a time of ah-ha moments all over the place. No one had all the answers about tongue tie and their related issues, but many had theories. |
I dove in. I recruited other professionals as supports. We networked. We shared experiences. We re-evaluated. We want the best for families.
My job as an IBCLC is not the same as those other supports and professionals but I want to share some of my learnings and reflections. I know tongue ties cause a lot of issues. I will not deny that, but I will say that just “getting it snipped” or getting into a dentist for a laser revision isn’t a guarantee things are going to be resolved.
A really key piece I have acknowledged is how much better babies that are at an appropriate weight recover and catch on to breastfeeding post-revision compared to babies that are underweight or slow gaining, maybe gaining weight a little faster than what is called a slow gainer and who maybe is not getting much concern from anyone but still not growing on “their curve”. Doing a revision on these babies is something I really hesitate to do now and I won’t make a recommendation for revision until resolution has occurred in the weight department. This to me a really good reason to be working with an IBCLC before hand.
Another really important part to working with an IBCLC is to assessing milk supply. Babies respond to flow and without that flow, they just won’t want to try and improve anything. Add in a tongue tie and they just don’t care to breastfeed nicely or at all. If supply is low, again even with a revision, they just are not happy breastfeeders. Both this scenario and the above one make people say “the tongue tie wasn’t the issue” and sometimes add in that “they did the procedure for nothing”. Being able to get moms working on supply, which in turn can help the weight gain issue, if it exists, helps ensure that once they get those two factors sorted out, they are ready for revision and have a good foundation to make the revision successful. The pieces fall into place nicely and almost predictably. It also helps me be able to tell a mom a timeline for “when will this all be better”. I can help them set up a plan so they can see a means to an end, rather than “just keep trying, it will click soon”.
There is also maternal pain that is often a concern and should be addressed INDEPENDENTLY of a revision. Sometimes tongue ties cause pain, damage & trauma to mothers breasts and can be resolved with a revision, but ideally more should be done to address this instead of just waiting for things to get better. When we deal with the breast/nipple independently, it makes the revision seem significantly more effective.
Babies can have other factors/stresses affecting and influencing breastfeeding that are often identified by IBCLC’s or professionals who assess physical factors, like Chiropractors or Osteopaths. I also find when we resolve these issues first, or at least start working on them, that things get back on track faster post-revision.
Sometimes I am not consulted until after a procedure for a tongue tie has been performed. When I get called after, I can most certainly still help and we can get past these remaining pieces, it just is in reverse. What I find though, is it is all a lot more stressful for moms and families because they also have a cranky baby and after care exercises to get in, as well as possible pumping & supplementing, and perhaps appointments with the other professionals we work with. I personally think It is better when I can set up a plan in steps with one focus at a time. Once supply and weight is up, it is one less stress, so the family can handle the stress of the aftercare and extra needs of the baby.
I am also aware that some parents would rather not go through a revision at all and this is where my “Before Tongue Tie” experience and knowledge comes in. I say to the parents and myself, “what would we have done BTT?” Are there strategies that would be useful and address the concerns? Sometimes there are solutions that the parents are 100% ok with and will get the baby fed and minimize concerns. Sometimes all of those are tried and the revision conversation might have to happen again. This is where knowing the risks to the situation and knowing what else to watch for is important.
Tongue ties are a topic that people get really excited about from many different perspectives and I don't see that changing for awhile, but I wanted to raise the thought that we are in a place of breastfeeding right now that in the years to come will be a historical recollection. It might be known as something more eloquent than BTT but until then we can recall what it was like BTT.
I want to be *explicitly clear* that this is NOT about individuals. This is not about the idea or execution of such events. This is not about women supporting or not supporting women. This is not about businesses who chose to plan events. This is not about businesses who participate in events. This is fully about the sponsorship by the companies covered by the WHO Code. (and I promise you they all know about the WHO Code and how that impacts their relationships).
So, what is the WHO Code?
The purpose of the Code is to protect breastfeeding, to protect all mothers and babies, regardless of their desired feeding methods, and to prevent aggressive marketing practices that often interfere with mothers meeting their own breastfeeding goals. Infant formula, feeding bottles, and artificial nipples are the main products that fall within the scope of the Code. Breast pumps are not under the scope of the Code BUT some pump companies violate the code because they market bottles and artificial nipples. Again, the Code only applies to the marketing of these items–it does not affect whether they are sold or used. Confusing, right?
Confused? Of course you are!
Then we have to consider who are the "kid" companies and who are the "parents"? Companies who are owned by Code violators are considered the same as their parent company. You really have to dig deep to find out a lot of this info, but if you start goggling different brands of formula, medications, infant supplies, etc you start to see that there are a lot of kid companies and just a few parents. The parent companies, of course, want to keep their smaller companies WHO Code violating record clean so that health care workers who have to adhere to the WHO Code can still have relationships with these companies, while the parent company gains benefits. They can also give items and samples not covered by the WHO Code and maintain compliance. But in the end, they are still violators.
As an IBCLC, I need to educate people about the WHO Code and marketing. What I am encouraging people to do, all across Canada, is to just keep their eyes open a little bit to who is hosting events, who is sponsoring events, what is that relationship like, who is providing the educational piece & decide if the information being given is evidence based and helping mothers meet their breastfeeding goals or if the information might be slanted. You will see a large variety of how these events take place and some will be absolutely ok and some are going to have questionable practices.
This is not about you and it is not about me.
I want this to be heard by everyone because if the doula/nurse/doctor/pharmacist or IBCLC, asked to participate this time walked away, the companies will just go to find another one. This also applies to educational events for professionals so not only do we look down, we have to look up. I want parents to hear this so if they go to an event they can also see who is providing the funding for the event and the information.
Eyes open!
I am here again suggesting you keep again breastfeeding old faithful on the shelf! At bare minimum before taking fenugreek to help an unsteady to low supply, keep that bottle of fenugreek sealed until some further investigation as to why you might need something to boost supply is started.
I think “breastfeeding issues” are sometimes breastfeeding issues but I also think that often time struggling with breastfeeding is just a symptom of something else. Paying attention to your supply as an indiction of something else, might actually help you understand more about your body and its personal needs.
This is not to say there are not good herbal options for supply, because there are. It is matter of knowing what is happening with your supply and your body, your own unique challenges and having a health history taken or worked up, so that the right herbal for each individual can be chosen/suggested. It might just be fenugreek for you. But, there is a good chance there is something better.
I will also add that many mothers experience upset stomach, gassiness, loose stools, diarrhea, dehydration, low blood sugar & unpleasant body odour when taking fenugreek. Baby may also show similar symptoms.
Here are 15 things you might not already know about vernix:
- The formal name is Vernix Caseous. Vernix means varnish and caseous means cheese-like.
- It is a naturally occurring biofilm made in the last trimester of pregnancy.
- The first mention of vernix was in the Dunglison dictionary of Medical Sciences in 1846. 1846. Can you believe that? And here we think we are on to something new these days.
- Vernix is unique to humans.
- At the time of birth, vernix might cover the entire body of an infant or it might only be found in the body folds of the baby.
- Vernix might take on a more yellow, green or brown colour instead of the typical white colour. These colours might reflect intrauterine problems or fetal distress.
- Vernix is 80% water and 20% lipids and proteins.
- Vernix, combined with amniotic fluid, is swallowed by the fetus in utero & has a positive impact on gut development.
- Vernix acts like lubricate of the infant during delivery.
- Vernix is antimicrobial. It is an antimicrobial agent that protects against the bacteria filled environment of the mothers vaginal area. It provides an acidic environment on the skin which is believed to inhibit the growth of problematic bacteria.
- Vernix acts an insulator post delivery as the baby transitions into the outside world and helps babies regulate temperature. (This can continue for up to 5 days if left on the infant.)
- Vernix is a great moisturizer and has amazing wound healing properties (studies are being done on burn injuries).
- Vernix is believed to have antioxidant properties, which helps aids against the stressors of birth.
- Vernix blocks out meconium contamination of amniotic fluid.
- The National Association of Neonatal Nursing (NANN) and the Association of Women's Health Obstetrical and Neonatal Nursing (AWHONN) released a consensus statement that states “removal of all vernix is not necessary for hygienic reasons” and “vernix may provide antibacterial promotion and wound healing”. The World Health Organization (WHO) also recommends leaving vernix intact on the skin surface after birth.
I think we can agree vernix is pretty amazing.
The term lactation consultant or LC has become the known, accepted title for a professionals with expert knowledge in breastfeeding. They may work with moms and babies to address breastfeeding issues and concerns. They may also teach classes, assist with establishing breastfeeding one on one, and promote and protect breastfeeding through policy, procedure within health care and government.
Origin of the term “Lactation Consultant
The accepted term for “IBCLC” or International Board Certified Lactation Consultant in many geographical areas is "LC" or Lactation Consultant because, as you can see, that term is a mouthful.
“LC” is not trademarked and does not hold the professional standard like “IBCLC” does, so one will occasionally find a practicing LC who is not an IBCLC. Consumers (mothers and families) and other professionals (doulas and doctors) need to be aware of this.
As well, not all those who work as “lactation consultants” in health centres or breastfeeding support centres are IBCLCs. Some employers encourage employees to pursue the credential but don’t mandate it for employment. Many times, nurses with some basic breastfeeding education fill these jobs.
Why is this IBC part so important?
The International Board of Lactation Consultant Examiners (IBCLE) awards the title of International Board Certified Lactation Consultant to only the candidates who meet the comprehensive pathway requirements and pass an international exam. This allows IBLCE to establish the highest standards in lactation and breastfeeding care worldwide and to certify only the individuals who meet these standards.
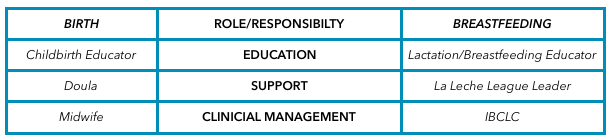 Breastfeeding education, support, clinical management
Breastfeeding education, support, clinical management Breastfeeding alphabet soup
I’d like to explain some of the breastfeeding alphabet soup by using the birthing support alphabet soup, as people seem to relate to that.
All the roles are important, but they provide their own distinct scope, responsibilities, and abilities. They can all work together to provide comprehensive support.
Primary roles of the individual bodies
As you can see, I’ve broken this down into three primary roles.
1. Education
2. Support
3. Clinical management
Education
Educators teach you about the normal and expected processes of childbirth and breastfeeding. They typically call themselves childbirth educators and lactation educators.
They teach the normal process of birth and what you can expect when having a baby, as well as encourage and promote breastfeeding.
This information helps you make decisions, helps you know if you are on track, gives you references for getting the birth and breastfeeding relationships you want, and helps answer your questions.
Educators typically teach community classes in group settings.
Support
Support people are typically those who have additional training in supporting mother, baby, and family during crucial times: birth and breastfeeding.
They’re typically doulas and La Leche League (LLL) leaders. Doulas are usually paid professionals, and LLL is a mother-to-mother peer support group. These roles offer the encouragement and motivation you need to get through the processes of birth and breastfeeding.
They are well versed in normal and expected outcomes. They know to watch for red flags to ensure they can guide you further if you have come outside the normal, expected process. Their job is to provide physical and emotional support, encouraging you to ask questions of your caregivers to make sure you’re well informed about what occurs. They have resources and guidelines to reassure you that you’re indeed in the realm of normal, and if things deviate from normal, they can point you in the direction of more resources.
Clinical management
Lastly, we have the clinical management professionals.
These are the folks responsible for the clinical and medical bits of the scenario. They look at the facts and figures, big picture, and red flags to rule in or out the things that are not in the normal and expected category and then make management plans from there. They have the clinical experience of things that fall outside normal and how to manage them.
Working together
All of these people have a place in the realm of support and caregiving; what’s important is they know their role and responsibility and respect the others’. Where it becomes problematic is when the client receives something different from what she expected to receive. Sometimes, this occurs because the roles of each provider isn’t clear to her, and she might conclude that one person isn’t performing a role properly. Let’s look at how this might apply to IBCLCs specifically.
In our example, a mother assumes that a breastfeeding educator* is an IBCLC. She notices that despite consulting with the helper, her breastfeeding issue remains unresolved. She decides to seek more help through a La Leche League leader, who determines that the issue is outside her scope and recommends an IBCLC. The mother insists that she already saw an IBCLC, but received no help.
*this person could also be staff at a breastfeeding clinic or nurse who comes to her home
This example is typical, and it hurts all support people. The educator gets a bad rep because she didn’t help. The LLL leader is helpless because the needs were outside her scope. The IBCLC profession gets a bad rep because the client misunderstood the different roles and expectations.
Clients need to know clearly what their expectations are and who can best meet those expectations based on role, scope, and experience. I want to be asked and welcome being asked these questions! I want you to go and look at the IBLCE website to see what IBCLC's are all about and verify I am indeed and IBCLC and see what scope and standards are laid in place for my profession. I welcome the same questions about being a doula! I would love to see a blog about midwives and how they are different from doulas and childbirth educators (wink, wink, nudge, nudge midwives).
All breastfeeding and lactation professionals have a responsibility to work together to ensure mothers have accurate information, so they can receive the support and encouragement they need as efficiently and as quickly as possible.

It is true that all over the place, in so many places new and expecting parents are visiting, there are posters and flyers and brochures and people encouraging breastfeeding and exclusive breast-feeding. This recommendation is world wide and comes from the World Health Organization. While I agree with all the benefits of breastfeeding, as most people would, it is NOT enough to just give benefits. In fact, it is dangerous to encourage and promote breastfeeding & yet not be able to follow through with the support needed. Breastfeeding is significantly more complex than the two-dimensional vision posters make it out to be. Most women are certainly not relating to the mothers on the photos of the breastfeeding books. You know, the mothers who have perfect skin, no bags under their eyes, pristine hair and makeup looking like they have zero cares in the world…beyond oxytocin highs.There needs to be support for the mothers that can breastfeed "easily" so they succeed. We also must meet the needs of and support the mothers in which breastfeeding is not going to work "easily" or perhaps not at all….and all the unique, complex cases in between this. Blanket statements are harmful, on all sides.
Supports for new families are getting less and less available and the resources we do have are not always adequately trained and skilled to handle the cases they have presented to them. For every mother who feels judged because she could breastfeed, but doesn't want to, there is another mother who is feeling judged because she wanted to breastfeed, but did not meet her goal. There are mothers who celebrate being told their babies need to be supplemented and welcome supplementation. There are mothers who are devastated when they are given the same news. We need to learn how to support all kinds of mothers and all kinds of scenarios. We have to be prepared for that to take more than 5 minutes in the doctors office.
Let's look at one way this all gets blurry. There are the mothers with babies who are not sleeping well but the mother has been reassured that this is just how breastfeed babies are. I don't believe that to always be the case…sometimes babies are not sleeping because they are hungry…breastfeeding is not working in that case, not for anyone. Mothers and babies need to sleep. Feeding endlessly for days and weeks is not healthy for anyone. The issue then becomes "exhaustion due to breast-feeding" weeks later, when breast-feeding issues could have been addressed, resulting in more sleep. Beyond that, families need support people to come in and do practical stuff, like care for a baby so mothers can nap, feed themselves, go for a walk. That doesn't mean breast-feeding needs to be discontinued, it just has to be understood and managed. Other examples would be a woman in so much pain from breastfeeding. Who wants to torture themselves 10 times a day. That is a breakdown waiting to happen. Again, lets get to the source as soon as we can. Get to the resolution so the mother can be pain free. There are so many options for that.
We know about postpartum blues and depression and how common it is. We also know that for many women it is so bad they are taking their own lives. It is horribly, horribly sad and devastating. I don't believe it is about mothers breastfeeding or not. I believe it is about support, or lack there of, about misunderstanding babies and mothers, about isolation and healthcare systems that seem to be set up for failure and not success, it is about misunderstanding what the Baby Friendly Initiative is and what it was intended to do and how it is supposed to work.
We can do better. We need to do better. Lives matter and are being lost.

One of the primary changes to the conversation is that we no longer can look solely at what is happening with the mother of the breastfeeding dyads, but we are looking at the baby also. I don’t mean positioning. I don’t mean skin-to-skin. I don’t mean early and often feeding. I mean, just as in how we look at a mothers ability to produce milk, we need to look at the babies ability to extract that milk. We know production of milk is primarily about supply and demand. Demand needs to be present first; this is the baby. Expulsion of the placenta stimulates the start of milk production & then the baby needs to drive it from there. If we are seeing something not working as expected, we need to assess both mother and baby. Often what appears as not working is “mom hasn't started to produce, her milk is not in yet, she just can’t produce milk or she cannot produce enough”. However, we then also say, and I am sure you have heard this, that very few women truly do not produce milk or produce lower amounts of milk. We use completely contradicting statements, loosely, but they are taken as hard, fast truths. Or we will say, “No, no, you are making enough for your baby. Of course, you are making perfect milk for your baby. Your body knows what your baby needs. Some babies are just slender. That is how breastfeed babies are. They feed all the time. They are slender. Babies on formula weigh more. Don't worry about it. Just keep feeding," Or have you heard about the mothers being told their breastmilk is made of water. They just don’t make “cream” like their friends. How confusing!
When the new growth charts came out, we expected to prove some of these theories .The new charts were based on breastfed babies, internationally, in favourable living environments. There is lots of history to read on the development of the WHO growth charts. In short, people expected to see breastfed babies being slender and slower gaining and waited to be able to say, “we, told you so”. Well, the laugh was on us. The new charts show that under favourable environments and feeding conditions, breastfed babies do weigh more than their formula fed counterparts and on the new charts breastfeeding concerns show up even sooner than previously. For example, it is common at a 4 month check up to see a baby on the old chart to not be gaining on the curve anymore. Now, with the new growth charts, that same baby would show up with less than ideal growth earlier, perhaps at 3 or 4 weeks. Growth failure was being seen as a normal negative deviation and being missed! It appeared almost as if advocates of breastfeeding were trying to downplay growth failure, because they so truly believed breastfeeding is the way to feed an infant and didn’t want to admit when it wasn’t working. I was fascinated by the charts and wanted to know why the data spread that way. (That could be my former career as a Medical Laboratory Technologist shining through).
About the same time I started looking at breast-feeding failure with my new set of lenses; the lenses that looked at mom and baby, not just a mother seemingly making too little milk, with pain or maybe without pain, with a screaming baby or maybe a sleepy baby, maybe a baby gaining weight but seemingly hungry all the time, maybe a baby with slow weight but seemingly content. I wanted to know more about all the babies & was learning more about babies. (What you seek you shall receive) I was introduced to the idea that babies cannot always function at the breast well, and therefore, the demand is not put on the mothers supply. Without demand, there is no supply! But can’t a mother just offer the breast more, get into bed for 24 hours for a breast-feeding vacation, do skin-to-skin, put baby in a wrap and walk and feed as baby needs and get that supply up? That is exactly what I was taught. Mom just needed to try harder and get supply up, drink more water, rest, take some fenugreek, drink lactation tea and eat lactation cookies. But, you know what? That wasn’t always working. Not with the cases I was seeing.
What i am not seeing is a change is how we see the idea of oversupply or overactive let down. If the idea of low supply is often being perceived incorrectly should we not consider the idea of overactive let down or oversupply isn't a true phenomena either? Could oversupply also point back to the baby? Is this another function consideration? I certainly think so. I would like to ask that we consider the let down and supply as normal flow, but, too fast for that particular infant. The infant, for varying reasons (and an assessment would be needed to determine the reason) is having a hard time controlling the flow of the milk. They choke, cough, sputter, leak milk, etc. They might have fast feeds, gain well and seem to adapt to this "overactive let down". As time goes on, supply decreases (we respond saying milk supply is now regulated as nothing was wrong anyway) and soon, the same mom with overactive let down, is saying she has low supply. WHY? Because the baby could not feed correctly from the beginning. They had difficulty at the breast, relied on that fast letdown and now without correct feeding behaviours, just like the low supply moms I talk about above, the demand is not there and so the supply goes down.
Something else we now know, that we used to say the opposite of, is that a hungry baby will cry and a content baby cannot be hungry, Regardless of weight gain plateauing on the curve, being slow gaining, so long as baby seemed content, no one worried. What we know how is that as milk supply goes down, appetite of the baby goes down. That appetite is the demand we need! So without the demand, we again will have no supply. This is quite a different tale than has been told in history!
Let's keep chatting! If you think you need some hep navigating your breast-feeding I am happy to book a time to see you and your little one.

I will also state that I and other IBCLC colleagues have witnessed mothers with supply issues that resolve after they stop taking placenta capsules. Again, this speaks to us not knowing the mechanisms behind how a placenta might aid or impact lactation.
In the end, my skill set as an IBCLC is of much more value than the time I would spend processing a placenta, in my opinion.
I do also have some personal hesitations that I wish for people to consider. I am not saying that they need to decide not to encapsulate after the considerations but just that they consider the points.
When we discuss postpartum mood imbalances & disorders we need to look at a larger picture than just a placenta. We see many mothers of multiples who state they did not consume their placenta after baby #1 but did after baby #2 and felt better emotionally than the first time. However, did they review the other differences? Baby #1 we often know little to nothing about what the experience of mothering will really be like, we go at it alone, we are not very confident in what we already know and we hesitate to seek out much information. Often baby #1 was a longer labour and longer pushing stage. Going from no baby to a baby, no sleep, constant physical and emotional demands from the infant, plus ones own recovery can be overwhelming. Baby #2, labour might be drastically different, maybe this time more supported, a shorter labour, easier pushing, the lack of sleep one gets with a newborn in the house is not as much as a surprise and there is much more understanding of normal newborn behaviours. Maybe the second time she had a doula, the same lady who encapsulated the placenta for her, and also provided postpartum supports, like helping with baby care so she could nap or helped with dishes and laundry so mom can rest, put up her feet and just focus on breastfeeding. Having some healthy meals with nutritional elements similar to a placenta might be a more regular occurrence the second time.
Speaking of nutrients; sometimes it is said that mammals consume their own placentas, so why wouldn’t humans? Some theories are that mammals do it for safety; that in the wild the smell of afterbirth would draw predators near and the mother & the newly born were vulnerable and at risk, so for safety, the mother would quickly consume the placenta. There are also some theories that a mother would be hungry and in the wild food is scarce. Their own placenta vs nothing was the best they could get so it could be considered a last resort for a nutritional deficient animal. We no longer live in the wild and food scarcity is not as prevalent. In this day and age, most humans don’t look at their placenta and see their next meal or have a desire to consume it. Even in the wild, they consume it mostly in one sitting and not small amounts over days and weeks like the placenta encapsulation community recommends now. Even with diminished nutrition in food sources, we can purchase vitamins and foods enhanced with vitamins, which could provide the same effects. There is a study I am aware of that is not yet completed and it does show that the mothers consuming their placentas do have higher hemoglobins at 6 weeks postpartum. However, it has also been commented that there is a chance that the families that have the available monetary funds to pay for placenta encapsulation services, also have the monetary resources to purchases better quality and quantity of foods. The cost of the placenta encapsulations has not been covered for the study. It is a control that needs to be considered.
As a former Medical Laboratory Technologist who worked in manufacturing of blood and blood products, I also worry about an appropriate environment to encapsulate and I do have concerns about infection control. I know that might be over-reactive but as someone who had to do quality control, sterility checks and saw the process of recalls, I think safety and specifications are important. I mean, after all, the placenta might be contaminated with poop. Even a small amount of bacteria can cause a big tummy ache. I say that more tongue in cheek than anything, but it is a thought. There is equipment needed to encapsulate and I am just not 100% that the risk of cross contamination is not there. Now, I am not an encapsulator and maybe there are steps in place to account for that risk. I am unsure about that. I am just saying, for me, it is something to think about. In the lab, in food processing, in other areas where contamination is a risk, sterility checks and quality control is what keeps stuff “clean and safe” and where recalls start, if they are needed. Just because you made the organ does not mean it cannot hurt you if bacteria is at play.
After all that, we do know that placebo effect can be strong and powerful. I am happy to accept placebo effect if you are and I am happy to refer you to a local placenta encapsulator if your desire is to encapsulate your placenta.

It is no secret I love essential oils. I really, really do. (I am a very committed doTERRA user) It is also no secret that I love helping moms breastfeed, to the point of making a living doing so. But, there are only a few people who know how much I dislike the use of essential oils for breastfeeding related concerns - like low milk supply or fussy, gassy, colicky babies. Surprisingly, it is not because I don’t think essential oils will help with those things. It is because there is almost always something more that needs addressing under those symptoms.
I am a huge advocate for alternative wellness. I think there are so many options out there for people to maintain optimal wellness and I am accepting of all sorts of options. However, I am also an advocate of knowing what it is one is dealing with when it comes to being off track from ideal wellness and I am especially passionate about this when it comes to babies. The truth is, there are very few people who understand lactation and so even when a mother sees a doctor who tells the mother she has “low milk” or “baby needs to be supplemented” they are not answering a very important question. That question is WHY? Why is the supply low? Why is baby not gaining as we expect?
Breast-feeding is the biological expected way to feed an infant, but sometimes it isn’t as easy as one would expect for such a natural act. There are so many reasons why mothers and babies struggle with breast-feeding. We could make a large laundry list of reasons although the little list would be not enough milk or it is/was too painful - sometimes both. Moms should know that they can look into it further & babies deserve that, too!
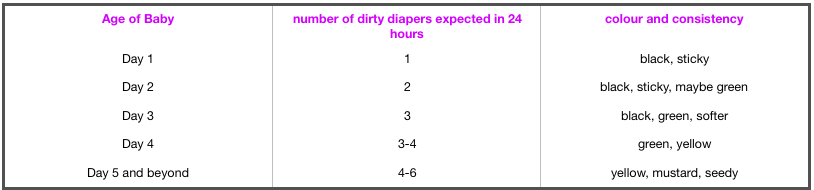
There are many reasons for complaints of low supply, weight gain issues, pain, and so many symptoms to tell us that breast-feeding is not working as smooth as it could be, or that baby is not feeling as well as a new baby should. I am thinking of things like sore nipples, low milk supply, low or no weight gain, a baby that is not seemingly full and happy, colicky, gassy, not pooping (YES, babies NEED to poop….disregard all the old opinions that breasted babies don’t poop frequently), not sleeping like a newborn (I don't mean to say babes sleep 8-12 hours a night and that is what you should be seeing. I am meaning naps and being able to be put down for little stints at a time vs a baby that is never settled & always falls asleep at the breast but startles as soon as he is set down).
These are all symptoms of a mother and baby that could use some help with breastfeeding. And yes, oils could help alleviate some of the stress and reduce the symptoms. I won’t say that they won’t help. But wouldn’t it be nice to figure out WHY this is occurring so that one doesn’t run into more troubles down the road? Using oils to help alleviate symptoms a little bit can make things seem better for a short time but in the long run can delay mothers and babies getting help they need and ultimately can end the breast-feeding relationship sooner than baby would like, and you better believe it, even sooner than a mother may like. When I work with moms and babies that are struggling to keep breastfeeding going and I do a history intake the dyads, so many times there are red flags in the early days. Most moms are told these are “normal” and not to worry, so they do not. We need to start paying attention to the first few days and weeks to make sure mothers are able to meet their goals of months and years of breastfeeding. Don’t just hand out some samples of myrrh for those sore nipples, or some fennel for that low supply or upset baby tummy. Get moms some samples in hand and do mom a favour and give her a recommendation for a solid lactation consultant (IBCLC) in their area to make sure that 1) the oils would be the right oil for what is going on and 2) help mom figure out why things are not working as smooth as they should be. In the end things are cause breast-feeding issues can also be affecting other areas of life for mothers and babies. Breastfeeding issues are not isolated to breastfeeding.
What if I told you could attend a 5 hour childbirth class? Yes, simply FIVE hours. There will be some homework, but I believe you are capable of doing this all on your own time. You will get from the homework what you put into the homework! I am there to help you with the homework, too.
Your Birth Experience is designed to connect YOU with all your childbirth options in a unique way. You won’t find a program like this anywhere else. It is comprehensive yet personalized to you.
In Your Birth Experience, there is CONNECTION to each expecting family, IDENTIFICATION of their individual needs, resulting in families being EQUIPPED to achieve their unique birth experience.
Everyone receives a copy of the YBE parent guide, complete with colouring pages. Yes, colouring pages. Colouring is a great activity in pregnancy & labour.
You will learn evidence based information on the process of childbirth and potential interventions.
You will envision your ideal birth experience and be provided with the tools that you need to make that happen. Note, that it is YOUR ideal birth experience, not mine, or anyone else’s.
You will learn labor comfort measures & relaxation techniques and we will practice them.
You will explore and discover your unique personality styles, how you tend to make decisions & how this affects communication.Communication is very important in labour and birth. You will be able to create a birth plan that effectively communicates your desires to your birth team. This helps you create the best environment for you and your birth team for your own unique birth experience.
We will also begin our entrance into the world of breastfeeding in this class. I say begin because there is a more in-depth breastfeeding class that is available. I have them broken into separate classes for a couple reasons - to help make more breastfeeding classes accessible to people taking other childbirth classes & your time commitment, you can break up learning sessions.
What won’t you find in this class? Videos of women giving birth. You are saying, “What? No videos? Why not?” I can tell you, that as a birthing woman, you will NOT be seeing or feeling birth from the angle or perspective that you will see in the video, so it might not be of any value. Another big reason is most of the support people we bring to classes with us do not want to watch birth, and also, may not be experiencing birth from that angle of perspective either. They are uncomfortable watching videos in a group setting and to be fair and honest, do not digest the content because they are distracted by the discomfort. Birth is a right brained activity, meaning we don't need to see birth to give birth. And another big reason, YouTube is full of birth videos. If you feel birth videos are important to watch, you have hundreds and hundreds available to you. You don't need me to facilitate viewings. We do, however, watch a video about breastfeeding. Breastfeeding is also a right brained activity however does have a left brained component to it, so it is helpful to see breastfeeding when preparing to breastfed.
You also will not hear about all the complications of pregnancy and/or birth. This is important for a few reasons. 1) I don't want to scare you. We will talk about fear in the class and how fear inhibits labour. 2) If you do have a unique concern in your pregnancy or birth, that is where your trusted care providers are your best resource, not your childbirth educator. I am a resource for you, for sure, but we do not need to discuss ALL the possible concerns, in order to understand the one or two you might be having. 3) Back to the communication I mentioned earlier in this post. I will help you to be able to communicate with your care provider so that you have all the info about your unique concerns. That is important. 4) There is info in the YBE Parent's Guide about possible complications and interventions, so you do have information. We just do not spend lots of time in the class because it doesn't universally apply to all.
I invite you to the next session of this class and am excited to help you prepare for Your Birth Experience. This class can also be done in your own home, one-on-one, if you prefer that option. Simply contact me to set that up!
Do you know what can mimic a tongue tie? Terrible breastfeeding technique can. The number one cause of many breastfeeding concerns or issues is positioning and latch. A good latch is vital to milk transfer. Good supply is dependent on milk transfer. Weight gain, pees and poops are dependent on supply. Swing back full circle to latch and latch is dependant on good positioning. This is true in the majority of cases. Add in that good positioning and latch should also make things easy, comfortable and pain free for mother. It should also make things easy, comfortable and effective for baby.
When we see concerns with breastfeeding we must start with full maternal and infant assessment. This cannot be skipped. This includes a history on the birth and the start of breastfeeding, how feeding has been going, any know medical issues that contribute to breastfeeding concerns with mom and baby, a feeding assessment including positioning and latch, and structural exams of both mom and baby.
Sometimes we have breastfeeding issues and concerns that are easy resolved by refining breastfeeding techniques. It can be that simple. Sometimes you will get breast-feeding technique (position and latch) perfect but there is still lots of trouble. We have pain, we have inadequate transfer, we have low weight, low pees and poops, etc. These are times we need to look further. There can be lots of reasons for this but today I am going to highlight tongue ties.
Tongue tie or poor breastfeeding technique?
I am all for fixing tongue ties. If they are a problem they are better resolved than to be “pushed on through”. However, I am more if favour of through assessment of breastfeeding & comprehensive follow up if a procedure is deemed warranted which is why I am drawing attention to this point today.
Assessment of breastfeeding MUST include watching a feed amongst structurally examination of mothers and babies. And we have to address position and latch. The sooner we do this, the better. Why? Because if we have position and latch causing pain and damage, it is hard to tell if position changes are helping the pain or not. If we have damage and trauma, even a good latch will hurt until that is healed. So, then if look at a baby and see what visually looks like a tongue tie, we start to get blurred lines. The simple presence of a frenum is not a tongue tie. Diagnosing a tongue tie requires more than just looking. It is an assessment of function. Now when we are dealing with breastfeeding infants that function includes transfer of milk, weight gain, position needs, maternal comfort, visual of babies like folds in the lips, blanching of the frenum, blisters in the lips, etc. The people that can assist us in revision of ties are doctors and dentists and I am grateful to have them as part of our team.
But, let me ask you how many doctors and dentists are watching feeds? How many would know how to throughly assess a breastfeeding session? How many know what to look for structurally in a mother? And throughly for an infant?
Doctors and dentists that we rely on in resolution of breastfeeding concerns by revising tongue ties are typically only looking for a tongue tie as the reason to why you are presenting themselves to them. Their brains are actually wired to look for a possible intervention to try and resolve the issues based upon their skill level, experience and ability to help.
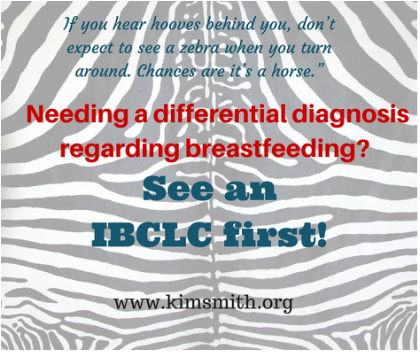
Have you heard this quote before? “If you hear hooves behind you, don’t expect to see a zebra when you turn around. Chances are it’s a horse.”
This means, first look for the simplest, common explanation to the problem presenting first. Once we have done this, then yes, we should go ahead and look for rarer & more problematic causes. In the medical community this is know as differential diagnosis.
How do you know what is causing your breastfeeding issues?
The most important key is to telling the difference between the horses and zebras. You cannot do this without a through evaluation, by a skilled practitioner. In the case of breastfeeding, these practitioners are International Board Certified Lactation Consultants. We have to be cautious of not assigning more importance to one element of breastfeeding than another, just because we think it is important or because we think the title of a certain practitioner is important or because that person thinks they are so important. There is another term for this which is “availability heuristic”. It is a bias towards things which you deem as more important because you readily recall it so deem it more probable. So, as someone looking at tongue ties most of the time this is front and centre in their minds. So, it is likely a dentist or doctor would go to tongue ties as a common cause of breastfeeding issues. As IBCLC’s we start at the basics, with the most common explanation of position and latch and move from there. The differential diagnosis mentioned about is what an IBCLC would do. This is why an IBCLC should be a first stop and why I think referrals for revisions of tongue ties should not be done without an IBCLC assessment.
I bring this up because I am seeing moms & babies after tongue tie revisions who I didn’t see before. I don't know what the baby looked like before but more importantly what I am seeing a little more frequently than what I would like is bad breastfeeding technique. I cannot help but wonder, if we had just corrected positioning, would that have been enough. Did we have a true tie or did we have symptoms of bad technique that are also symptoms of tongue tie. Looking back at the information presented above about assessments, evaluations, horses and zebras & availability heuristic people you can see where my concern is warranted.
Where do you go from here for support in resolving breastfeeding concerns?
Be wise in your selection of care providers when you are struggling with breastfeeding. Step #1 should be an assessment with a skilled IBCLC. From there we will make all appropriate referrals to other members of our team that assist with getting breastfeeding back on track. If you are in Regina or in the Regina area, I would be happy to help you navigate your breast-feeding challenges. You can give me a call or easily book online.

Sore nipples can be one of the more common breast-feeding challenges. You certainly are not alone in this, however, you don't need to remain sore, or worse yet, in pain. Pain at any point is your bodies way of telling you something is wrong and you need to pay attention to yourself.
What causes soreness and pain?
Most commonly it is because of trouble with positioning and latch, creating friction, and proceeding them to soreness, cracks, blisters, bleeding and sometimes infections and even lose of skin.
What can be done? Here are a few quick ideas.
Most importantly, check your position and your comfort. One of my rules is to make sure mom is comfortable first. Ideally, mothers are slightly reclined, arms and shoulders lose and down, and her neck has the ability to be relaxed. With this, mothers can then bring baby to them. You don't want to try to take your breast to baby. Baby can be front-to-front with mom, being supported by mother’s arms, and mother’s arms can be supported with pillows. Use gravity to help baby get on the breast deeper, rather than sitting upright and having gravity pull baby down or away from the breast.
If we still have discomfort, we need to check baby’s latch. A good latch is vital to comfort but also to long term duration of breastfeeding. A good latch is key to effective feeding which is essential for adequate milk supply. You might need to ask someone for help with checking the latch. If someone tells you it looks good, but you have pain during or after a feed, you need to ask someone else.
If position changes do not help with latching issues and soreness and pain are still prevailing sometimes we need to look farther into reasons and makes plans. Sometimes we can use a nipple shield to help protect the nipple and help baby to latch. It is important to get good help if needing a shield. There are important things to watch for such as fitting, proper placement, adequate milk transfer, babies output and weight gain. This is very important to know and recognize however; nipple shields are a Band-aid solution. They are not an answer, they are simply a tool to help keep the baby breastfeeding, at the breast, rather than quitting breast-feeding or going to pumping and feeding another way. It is a short term tool that needs a bigger plan.
Throw away the lanolin! For years we were told Lanolin was fabulous and all new mothers needed it. But the new research shows us, doing nothing is actually more effective than lanolin and in fact lanolin can delay healing, making things even worse for a longer period of time. Mor effectively you can apply breastmilk to the nipple or coconut oil or calendula if you want to try something else.
Do not let you nipples be wet and cold at the same time. Again, we were told for years that we should let the nipples air dry. But for mother’s with very sore, damaged nipples, the cool air can cause more harm. It is a good idea to apply heat while the nipple dries. Something like a rice sock or heating pad after baby unlatches, or even when getting out of the shower or bath, can help. This helps bring blood flow to the nipple that previously was restricted.
Soreness and pain are not considered normal for breastfeeding at any time or for any length of time. If basic positioning and latch changes do not help, it is worth having someone skilled come and have a look. They can help assess and evaluate what might be happening and help you make a plan to further overcome the struggles.

A couple brought their very ill young infant to the emergency room. I was called down to do blood work which was standard procedure. After having a difficult time drawing the blood I returned to the lab to run the tests & analyze the results, hoping to shed some light on why this infant was so ill.
Some of the initial tests gave results that led to further testing. One of these further tests was a “blood smear”, where we smear blood onto a slide and look at it under a microscope. As I was looking at the smear, I started to think that something was wrong with my equipment or my reagents; something was greatly wrong. My blood smear looked like something I had never seen before. I made a new slide and the same thing happened. I changed all the reagents that could be contributing to the bizarre results. each test gave the same outcome. I needed to accept that this was how this child's smear was. This told me why he was so ill. The baby’s treatment continued. Testing continued. My shift ended.
I returned the next evening still thinking about this infant and wondering if we had any more answers. I wasn’t prepared for what I heard and couldn’t believe it when I heard it; the infant has passed away, and the cause of death was malnutrition. He had been fed Coffee Mate and water in place of infant formula. I asked myself, as you may be asking yourself, how does this happen?
It turns out it happened, because the family became dependent on the food bank for food, including infant formula. When there was a shortage of infant formula, the parents decided to substitute with Coffee Mate and water. Some will say that it was because they were illiterate and didn’t know the difference. Some would say it was because it resembled infant formula. Some will say it’s because a milk-like product equals milk-like product.
This experience stays with me, and I reflect on and react to the action of infant formula being distributed at the food bank. Food security is a basic need, and, for an infant, it’s one of the few things they need and they need often.
How does formula get to the food bank? Often the samples that are sent to new parents end up there. Women who choose to -and successfully- breastfeed then have these cans and bottles of formula sitting in their homes in dark cupboards, on top of the fridge, and other out of the way places. They know they will never use it, but the idea of letting it go to waste or ending up in the garbage isn’t something they want. They think about all the moms who have less than they do, less support to breastfed and use the food bank - and think that if they take it there, they can help a mom. Moms who need the food bank go there, they say that formula is available, and they take it. That helps the family budget. Formula is expensive and is likely a large part of the financial stress of the family. What’s wrong with that? The samples don’t come consistently and frequently enough to sustain the food bank supply. There will be times when the food bank doesn’t have a supply of formula but the mothers are assuming it will be available so the income gets budgeted to other items. Now, the food bank has no formula, and the family has no money. They still need to feed the baby.
In my ideal dream world, the supports these families would receive would be breastfeeding support as well as prenatal and postnatal education. Breastmilk is virtually free. With even suboptimal nutrition, mothers still produce a perfect, free food for their infants. Infants can be sustained for a significant amount of time on just breastmilk.. The recommendation from WHO and CPA is 6 months exclusively and then continued to two years or beyond, with the introduction of solids at around 6 months. In the event of a food crisis, a mother could sustain her infant for the better part of its first year through breastfeeding alone.
The support aspect would be important for that to happen. These mothers also need the education. Many of them believe that without an optimal diet, their breastmilk isn’t good for their baby and that formula is better. All mothers want the best for their babies. They need to be taught that they’re what’s best for their babies. They also need to be taught what normal infant behaviour is. If they don’t understand normal infant behaviour , they may feel like they’re starving their baby. Without access to infant formula, they would likely plug along and make it work. With formula being free and on the shelf at the food bank, however, they may grab it and feed that to the baby. Many of us know, when we start supplementing, we can quickly lose that breastfeeding relationship. The food bank may continue to have formula or they may not and we end up in situation like the above. How do we feed the baby in this situation?
The staff at the food bank could use some education on breastfeeding and formula feeding. Many of them may still hold the belief that mothers with a low-quality diet shouldn't breastfeed, that it isn’t good for them or their baby. When formula is available, they may encourage that to a mother who’s breastfeeding because of this belief.
Don't get me wrong here; the issue isn’t the people donating the formula to the food bank. They have good intentions and likely don’t realize the damage that can be done. The issue here is that this is exactly one of the things the formula companies want to happen. They want their products in the hands of the vulnerable new mother and father. This is why they send packages out, and they do it in the manner of “Breastfeeding is best; however when the time comes, introduce formula”. If the time comes to introduce it and continue with it, you will buy the kind that was free and came with coupons and other swag items like a backpack or change mat. It’s all marketing. How free do you think all that stuff was to produce and mail out? Not free at all; in fact, it’s in the high price of the formula. Let’s look at what formula is and why it costs so much. Those sending it out are a business and they need to make a profit. After all the free packages they give away, they need to increase the cost of formula drastically to make a profit. They’re so profitable, in fact, that not only are they giving parents free stuff, they buy the names and contact info of parents from the likes of maternity stores and giving all kinds of free stuff to hospitals and doctors’ offices. When a family legitimately needs formula, it’s so drastically overpriced that it creates hardships for them.
What do I suggest we do with the free samples? I suggest they be returned to the stores where they came from with a note explaining why it’s being returned. Imagine if just a small percentage of moms did this. Would the stores start to think twice about their partnerships if they had a large number of packages to deal with?
Another option is return to sender. I don't think this would have near the impact as the above option, but it would show them that you don’t want their products.
As far as the moms who need the additional supports and are at higher risk of needing to use formula, there’s a better way to help those mothers feed their babies safely and reliably.
This should go without saying, but the need to say it is always there. This isn’t about formula vs breast milk, nor about a mother’s choice to breastfeed or not. This is about an infant’s right to quality nutrition and food security, one of the basic hierarchical needs of the human race and a primary building block of children's futures. Breastfeeding can almost always guarantee an infant and child can be sustained.
I am going to highlight a few. If you think of others that could be added, by all means leave a comment and I will add them in!
1) We, the client and myself, have a mutually agreed upon, prescheduled time. Free clinics often have you come in, take a number & sit and wait for your turn. They won’t likely know how many moms are going to show up, meaning mothers & babies (maybe fathers and other children,, too) could wait for quite some time and then be feeling rushed. They see all the other moms & babies waiting for their turns. At the centre we have a scheduled time, hopefully to your convenience and we allow enough time to avoid feeling rushed. Home visits provide a scheduled time AND the privacy and convenience of your own home.
2) I simply have more availability and flexibility. Not only is the timing better but you get more options as to when. Again, free clinics might only happen once a week. What happens if your struggles start on the evening the free clinic was being held and you missed it? Or sometimes you may benefit from two appointments only 2 or 3 days apart. A week can seem like an eternity when you are struggling.
3) I am an Internationally Board Certified Lactation Consultant (IBCLC). Not all the staff at the free clinics may be an IBCLC. The free clinics are staffed by Public Health Nurses (PHN's). Some PHN’s are IBCLC’s but not all are. I am an IBCLC dedicated solely to breastfeeding, with 10 years of experience helping moms and babies, 5 years as an IBCLC. (By the way, if you use the free clinic, don't hesitate to ask if the person helping you is an IBCLC. If you really wanted to, you could consult the IBCLC directory.)
4) Education is a high priority to me. I mean MY education and I mean YOUR education. I have attended, and continue to attend, a wide variety of additional & extended trainings and conferences. I have a strong ethical background to practice evidence based lactation “science”. I also want to give you enough information about what is going on with you and will answer all the questions you have. We book enough time to be able to do this.
5) In all my years of experience I have had access to ranges of breastfeeding from normal to extreme difficulties. My initial exposure to breastfeeding help was a peer-to-peer support group where our scope of practice was to help mothers by providing emotional support & information within “normal” breastfeeding. I got to know normal really well and be introduced to some not so "normal". I was super curious about those not-so-normal cases and pursued my IBCLC. Now I have much more training with the outliers of normal. I am also able to follow my own client cases much more closely to monitor outcomes and refine the plans along the way. This gives me the advantage to know whether the information and care plans I am sharing with clients really work. Often in a free/public setting you will be exposed to different staff member every visit and they do not have that same luxury. They might tell all the moms to do the same “thing” thinking it is best practice and not realize that is not useful for moms to do and they are not getting the desired outcome.
6) I have direct access to centre physicians if something is outside my scope of practice or comfort zone and we want or need a physician involved on some level. This is especially useful for further diagnostic testing or prescriptions we might want to consider. We have developed some great protocols together and collaboration like this is unique, yet so beneficial and much more efficient for resolutions of concerns.
7) It is my standard practice to do a through history of mother and baby. We need to make sure that we have all aspects and contributing factors considered when we are determining why there might be struggles. There are more factors to lactation than most people are aware of. I go much further beyond getting a better latch and a better position. We make sure to look at the situation from a few lenses. We pull out the puzzle pieces that might be problematic and piece by piece get the whole puzzle fitting together into a nice picture.
You should hopefully be able to see what we are offering is completely different from what is being offered for free. You can count on focused, one-on-one care with a plan to approach the issues that brought you to me. You have the opportunity for follow up with the same person you saw originally and someone that can dialogue or report back to your physician and other care providers. I can help you address the specific concerns you have and reassure you what is the normal course of breastfeeding and give you my expertise with the more challenging aspects, with references and resources from the latest research. I can also make referrals and recommendations easily to a variety of other health care practitioners who may be of value to your specific concerns.
I look forward to seeing all of you and your darling little ones. Please feel free to book an appointment at your convenience.

Why are only a quarter of babies getting any breastmilk by the middle of their first year? A very large part of it is that there is a fabulous amount of interference. Interference comes from all over and starts long before babies are even born. Dare I say this interference starts before most babies are even conceived? Let’s look at media. Let’s look at the propaganda all over medical establishments, directed both at patients and at medical professionals. Let’s look at our own communities and then our own families. What is the message out there reaching people? Could this be part of why we are not able to help remedy breastfeeding?
They are certainly not breastfeeding friendly messages. But, let’s say you get through all of that and to the people that are supposed to be promoting and supporting breastfeeding. You know what? You still will here a large amount of variants in what these people say and recommend you do. From basics of position and latch to troubleshooting concerns, it seems very few of us on are the same page. It is highly frustrating as a professional and I know it is highly frustrating as a parent. It honestly makes me ask myself, what do we know about breastfeeding?
For many years I was involved with a peer support group. Within this group I was told that this is where we see normal breastfeeding. It was a well-established group with many, many years of experience in breastfeeding. This was my introduction to breastfeeding outside my own experience and being able to view and witness many dyads and what breastfeeding looked like for others. It was amazing and eye-opening. I learnt lots and went on to learn more and become a peer-volunteer to help mothers that were struggling. I was all in. Consuming all I could to try and figure out the barriers to successful breast-feeding. I had a big blue book full of breastfeeding information. I studied it. I did activities and exercises to help me expand topics. I read and read and discussed breastfeeding at great length. I was accredited and able to start helping moms. Moms would call me with concerns and I would look up moms concerns and then read to them from the book what the strategies were to help them overcome their challenges. I very often never heard back from these mothers to know if things resolved or not. I am hopeful many mothers did better and were successful but I know now that lots did not. I saw many moms in person return to meetings month after month and got to know many of these dyads well.
We told mothers what they could do right to make breastfeeding work well and especially how if people didn’t interfere all would be good for them. Feed early and often and supply would be there. Don't have pain meds in labour and baby will breastfeed well. Stay away from bottles & supplements and pacifiers and just feed and feed and feed. Yet, that didn’t work for everyone. I really was perplexed as to why. After a few years of this, that is when I decided to expand my education and knowledge and scope of practice. I was going to pursue being an IBCLC. I mean, I knew normal breastfeeding, right? How hard could it be?
Was becoming an IBCLC easy? Not at all. Was it hard? Yes, indeed. On so many levels. I was shocked when I started getting assignments back with really low grades. So many wrong answers. But how? I KNOW breastfeeding. I have been helping moms for years. I have these answers in a big blue book. It says here in black and white this is how breastfeeding works and this is what you do to overcome the struggles. It was wrong? How could it be wrong? How many women did I tell this info to? And how many of my friends did what the book said. This is how breastfeeding is, this is the normal for breastfeeding and all moms and babies are different and that’s ok. But I came to learn, yes, some concerns are common but there are actually tighter perimeters on what is “normal” and expected. I was pointed in a new direction for learning. My beliefs shifted in a few ares. Change is hard. But I was changed. I started seeing stuff in different ways, through many different eyes, many different versions and was taking a critical look at what I knew and what I was learning and the work of many others.
I learnt about growth charts and poop (oh how I love to talk poop now), infant sleep, tummy time, newborn weight gain and loss, milk supply, medications, medical conditions, how to supplement and when it actually is helpful, and how much happier and less stressed some moms and babies (and their families) could be and how to screen the bigger picture. I learnt more than how to tell moms more than “this too shall pass” & “some babies are just like that”.
I also learnt that professionals don't agree on a large number of topics. Weight loss, sleep, pain, creams, positioning. When and why did someone decide that 7% loss if ok, but 10% means we must supplement? Why do some think there should be zero weight loss at birth and some think it is acceptable to take 2 or 3 weeks to get back to birth weight? Why do big babies need to be supplemented an hour after birth but small babies are ok? Why do some say that sore nipples is a right of passage and some think there should be no pain, ever? Why are some nursing babies like footballs and other think we rarely should do this? This list could go on and on.
For some of use we come to our own conclusions based on clinical experience and patterns and outcomes that we see. Some of us just read the guidelines laid out for us because that is how it has always been done. Some of us are halfway between. Some of us come from a place of our own experiences and judgement and biases that come from that. (The latter is really not best practice and we need to learn how to detach from our own experiences to look at the current evidence in front of us.) Some of started in one place and have landed in another.
I can say that I believe I do have good evidence based research to back my opinions on many of those questions, plus many others. I have protocols and practices that I use over and over with success with families, but am happy to say as much as they are protocols they are very flexible and can be defined differently for each family. I haven't stopped seeing stuff in different ways, through many different eyes, many different versions and haven't stopped taking a critical look what is happening with my clients and figuring out how I can best help them met their goals.
Kim Smith
IBCLC,
Chatting about a variety of birth and breastfeeding topics.
Categories
All
Breastfeeding
Breastmilk Donation
Childbirth
Doula
Essential Oils
IBCLC
Lactation
Low Supply
Pain
Postpartum
Sleep
Thrush
Tongue Tie
Vasospasms
Weight Gain
Archives
September 2023
May 2022
September 2021
July 2021
February 2020
January 2020
April 2019
February 2019
January 2019
December 2018
October 2018
August 2018
June 2018
April 2018
September 2017
August 2017
April 2017
February 2017
January 2017
September 2016
August 2016
July 2016
June 2016
April 2016
March 2016
February 2016
December 2015
November 2015
October 2015
September 2015
August 2015
July 2015
May 2015
March 2015
February 2015
January 2015
November 2014
May 2014
April 2014
March 2014













 RSS Feed
RSS Feed
