|
The term lactation consultant or LC has become the title for someone with expert knowledge in breastfeeding. They may work with moms and babies to address breastfeeding issues and concerns. They may also teach classes, assist with establishing breastfeeding, and promote and protect breastfeeding. Origin of the term “Lactation Consultant The term “LC” originated as a short form of “IBCLC” or International Board Certified Lactation Consultant because, as you can see, that term is a mouthful. “LC” is not trademarked and does not hold a professional standard like “IBCLC” does, so one will occasionally find a practicing LC who is not an IBCLC. Consumers (mothers and families) and other professionals (doulas and doctors) need to be aware of this. As well, not all those who work as “lactation consultants” in health centres or breastfeeding support centres are IBCLCs. Some employers encourage employees to pursue the credential but don’t mandate it for employment. Many times, nurses with some breastfeeding education fill these jobs. Why is this IBC part so important? The International Board of Lactation Consultant Examiners (IBCLE) awards the title of International Board Certified Lactation Consultant to only the candidates who meet the comprehensive pathway and pass an international exam. This allows IBLCE to establish the highest standards in lactation and breastfeeding care worldwide and to certify only the individuals who meet these standards. Breastfeeding alphabet soup I’d like to explain some of the breastfeeding alphabet soup by using the birthing support alphabet soup, as people seem to relate to that. All the roles are important, but they provide their own distinct scope, responsibilities, and abilities. They can all work together to provide comprehensive support.
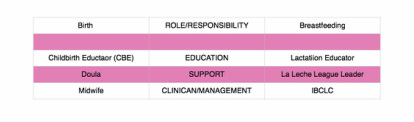
Primary roles of caregivers As you can see, I’ve broken this down into three primary roles. 1. Education 2. Support 3. Clinical management Education Educators teach you about the normal and expected processes of childbirth and breastfeeding. They typically call themselves childbirth educators and lactation educators. They teach the normal process of birth and what you can expect when having a baby, as well as encourage and promote breastfeeding. This information helps you make decisions, helps you know if you are on track, gives you references for getting the birth and breastfeeding relationships you want, and helps answer your questions. Educators typically teach community classes in group settings. Support Support people are typically those who have additional training in supporting mother, baby, and family during crucial times: birth and breastfeeding. They’re typically doulas and La Leche League (LLL) leaders. Doulas are usually paid professionals, and LLL is a mother-to-mother peer support group. These roles offer the encouragement and motivation you need to get through the processes of birth and breastfeeding. They’re well versed in normal and expected outcomes. They know to watch for red flags to ensure they can guide you further if you have come outside the normal, expected process. Their job is to provide physical and emotional support, encouraging you to ask questions of your caregivers to make sure you’re well informed about what occurs. They have resources and guidelines to reassure you that you’re indeed in the realm of normal, and if things deviate from normal, they can point you in the direction of more resources. Clinical management Lastly, we have the clinical management professionals. These are the folks responsible for the clinical and medical bits of the scenario. They look at the facts and figures, big picture, and red flags to rule in or out the things that are not in the normal and expected category and making a plan from there. They have the clinical experience of things that fall outside normal and how to manage them. Working together All of these people have a place in the realm of support and caregiving; what’s important is they know their role and responsibility and respect the others’. Where it becomes problematic is when the client receives something different from what she expected. Sometimes, this occurs because the roles of each provider isn’t clear to her, and she might conclude that one person isn’t performing a role properly. Let’s look at how this might apply to IBCLCs specifically. In our example, a mother assumes that a lactation educator* is an IBCLC. She notices that despite consulting with the LE, her breastfeeding issue remains unresolved. She decides to seek more help through a La Leche League leader, who determines that the issue is outside her scope and recommends an IBCLC. The mother insists that she already saw an IBCLC, but received no help. *this person could also be staff at a breastfeeding clinic or nurse who comes to her home This example is typical, and it hurts all support people. The educator gets a bad rep because she didn’t help. The LLL leader is helpless because the needs were outside her scope. The IBCLC profession gets a bad rep because the client misunderstood the different roles and expectations. Moms need to know clearly what their expectations are and who can best meet those expectations based on role, scope, and experience. All breastfeeding and lactation professionals have a responsibility to work together to ensure mothers have accurate information, so they can receive the support and encouragement they need as efficiently and as quickly as possible. In 2012, Finish researchers published a study in the Journal of Clinical Nursing reviewing past studies that had “focused on breastfeeding, breastfeeding support interventions, and education of healthy mothers and infants”.
The researchers combed through 34 studies published between 2000 and 2008 that were focused in Europe, North America, Australia, and New Zealand. At the time they began the study, the researchers pointed out that peer breastfeeding support was rising in popularity, particularly in the UK. Even so, very little research had been done up to that point on peer support, its cost effectiveness, and its impact on breastfeeding rates. Researchers outlined 4 elements that are necessary for peer support interventions to be effective: 1. Well-planned peer education Mothers were generally dissatisfied with the support of their peers if they had received no training. 2. Continuance of support from pregnancy to the postpartum period If new mothers receive no support during pregnancy or at the hospital, any postnatal support would likely be ineffective. 3. Working together with professionals Professional support is critical while the mother is at the hospital and if she experiences serious difficulties while breastfeeding. On the other hand, peer support can better offer advice related to breastfeeding and everyday life. 4. Variety of means to give support This includes such things as individual support, support groups, educational classes at the hospital, hospital-based breastfeeding drop-in centres, pictures, and breast pump loans. The most important requirement for ensuring a successful breastfeeding experience is that the mother feels supported and empowered. Because support must happen over a period of several months, having a variety of trained support persons is integral. It’s unreasonable to expect that a friend, mother, or even a doctor will be able to provide continual support for such a long period. Having a team—no matter how loosely based—can help spread out the burden of supporting a struggling mother. In addition, hiring a lactation consultant can be an ideal combination of peer and professional support. Lactation consultants are educated and trained; they are available for prenatal, natal, and postnatal support in a comfortable and approachable manner; they work with professionals, and they have access to a variety of support methods. Contact me if you’d like to know how I can provide the best support you can receive. |
Kim Smith
|
 RSS Feed
RSS Feed
