|
“You need to nurse for 20 minutes on the first side and then move baby to the other side for twenty minutes.” or "You have to empty the first breast before going to the second breast". Did anyone ever tell you these things? What if your baby only nursed for ten minutes? Did you ask what would happen? I suspect you may have been told that is not long enough for your baby to get the hindmilk (higher fat milk). Is 20 minutes that magic “long enough” time frame? What if baby wanted to be there for 25 minutes? What happens then? Do you have no more milk? Have you ever expressed breastmilk? What does it look like? Have you expressed more than one time? Did your milk look the same each time? I suspect it varied from thin, watery and blue, to yellow and thick. Did you notice a difference with the time of the day you pumped? How about before a feed or after a feed?
What does the research say? In point form the basics are: · As the baby feeds the content of the milk the baby receives is higher in fat · Each feeding can vary in fat content over the course of the day · The fattiest part of one feed might actually contain the same fat content of the start of another feed · Milk is milk; no real need to differentiate foremilk and hindmilk. Some is more concentrated, some less so, but your baby needs it all.(Hindmilk would be better called "concentrated milk" and foremilk "dilute milk") · Babies all stay at the breast for different lengths of time and what satisfies them varies · The breast is not a reservoir. It is never “out” of milk. If babe hangs out nursing more milk will “let down”. If you switched breasts milk may flow faster because more milk is in that breast, but there is no rule to have to take a baby off one side to put him on the other because of foremilk and hindmilk. Yes, if we want "moremilk" Is there a time when we might pay more attention to foremilk and hindmilk? · Is there an issue with baby sleeping at the breast? · Is there an issue with baby being fussy at the breast? · Is there an issue with babes weight? · Is baby swallowing at breast? · Is baby relaxed, with wide open hands and content at the end of feeds or no? If there are any of these types of concerns, seek out an IBCLC to address the concerns. It may be somewhat related to the so called foremilk/hindmilk. It can sometimes be ONE factor to take into account for the whole picture when some of the above issues are seen. But it would not solely be a foremilk/hindmilk issue. Many mothers will be able to relate to this experience. The experience looks the same; a routine infant check up appointment, baby gets a weight check, the parents are asked some questions about development, etc. Upon looking at the weight, it is determined the infant is not gaining weight as expected. What does this mean? What is the cause? What should be done? It often is quite shocking to parents, especially mothers, to hear this news. They are perplexed because they thought feeding, usually breastfeeding, was going ok. How is it possible that baby isn’t gaining weight? How is it possible she didn’t know that baby wasn’t growing as expected? Can anything be done? Common reasons provided for this phenomena is that mom has low milk supply, baby isn’t getting enough hind milk or baby is too sleepy and isn’t feeding often enough. I don’t think it is quite that simple.
What I find in these scenarios, because I get calls often after an experience like this, is that what is not communicated to the parents is why we do these checks, why they matter, what they mean and what should be done with the information. The simple answer is that we expect babes to maintain their own curve that they plotted on at birth (or more ideally 24 hours). When babies start to drop off that curve, this gives us a sign to look and assess what might be happening. This is a clue to ask some more questions and see if there are other pieces that can help tell us what might be happening. We want to know more about feeding behaviour, mood, output. Often what I hear is that there is no way baby needs to eat more. They are happy, content, sleep well, don’t really fuss. The opinion is that there is no way it is possible the baby isn't eating enough. People expect a hungry baby to cry, be irritable, to unsettled. I am going to say this is simply not true. I am sometimes more concerned about that “good baby” that sleeps well and always content. A very misunderstood piece of infant wellbeing is that weight gain influences appetite. What I mean by that, is that if a baby is gaining well, they demand to fed and show signs of being hungry regularly with easily identified feeding cues. What we think is a content baby because they have a calm mood, could be a baby who is content but not getting quite enough intake. A baby that is lower weight than expected, will have a lower appetite and will in fact cue less to be feed, will have subtle cues, likely won’t have a late hunger cueing & overall may make little fuss about it. If mother offers they will feed, but commonly have short feeding sessions. When they are being feed, their appetite is low so they do not do an efficient job, leading to milk being left in the breast and the body slowing down production. I give the example that if they are getting 70% of their intake requirement, they will eat at 70% efficiency (this will very baby to baby). This over time can cause a low supply, which influences their feeding because babies like flow...so low flow, means less interest in feeding and the cycle continues. If none of that concern is explained to a family, they leave these routine visits confused and bewildered as to why some one had a concern or what they could/should do about it and have no idea why it happened in the first place. There are lots of factors to consider to understand why this is happening & what the appropriate action for each case should be. If you are experiencing a difficult feeding situation where weight gain is a concern, booking a consult with an IBCLC is advisable. With a good assessment by an IBCLC, the root cause can often be determined and a solid plan can be put into place to get the baby fed, get weight gain concerns addressed, increase milk supply, maintain breastfeeding, etc. Other things to note in cases of lower than expected weight gain could be:
What is a Lactation Consultant, LC, IBCLC? The term lactation consultant or LC has become the known, accepted title for a professionals with expert knowledge in breastfeeding. They may work with moms and babies to address breastfeeding issues and concerns. They may also teach classes, assist with establishing breastfeeding one on one, and promote and protect breastfeeding through policy, procedure within health care and government. Origin of the term “Lactation Consultant The accepted term for “IBCLC” or International Board Certified Lactation Consultant in many geographical areas is "LC" or Lactation Consultant because, as you can see, that term is a mouthful. “LC” is not trademarked and does not hold the professional standard like “IBCLC” does, so one will occasionally find a practicing LC who is not an IBCLC. Consumers (mothers and families) and other professionals (doulas and doctors) need to be aware of this. As well, not all those who work as “lactation consultants” in health centres or breastfeeding support centres are IBCLCs. Some employers encourage employees to pursue the credential but don’t mandate it for employment. Many times, nurses with some basic breastfeeding education fill these jobs. Why is this IBC part so important? The International Board of Lactation Consultant Examiners (IBCLE) awards the title of International Board Certified Lactation Consultant to only the candidates who meet the comprehensive pathway requirements and pass an international exam. This allows IBLCE to establish the highest standards in lactation and breastfeeding care worldwide and to certify only the individuals who meet these standards. 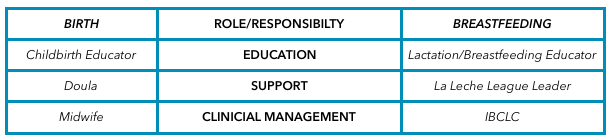 Breastfeeding education, support, clinical management Breastfeeding education, support, clinical management Breastfeeding alphabet soup I’d like to explain some of the breastfeeding alphabet soup by using the birthing support alphabet soup, as people seem to relate to that. All the roles are important, but they provide their own distinct scope, responsibilities, and abilities. They can all work together to provide comprehensive support. Primary roles of the individual bodies As you can see, I’ve broken this down into three primary roles. 1. Education 2. Support 3. Clinical management Education Educators teach you about the normal and expected processes of childbirth and breastfeeding. They typically call themselves childbirth educators and lactation educators. They teach the normal process of birth and what you can expect when having a baby, as well as encourage and promote breastfeeding. This information helps you make decisions, helps you know if you are on track, gives you references for getting the birth and breastfeeding relationships you want, and helps answer your questions. Educators typically teach community classes in group settings. Support Support people are typically those who have additional training in supporting mother, baby, and family during crucial times: birth and breastfeeding. They’re typically doulas and La Leche League (LLL) leaders. Doulas are usually paid professionals, and LLL is a mother-to-mother peer support group. These roles offer the encouragement and motivation you need to get through the processes of birth and breastfeeding. They are well versed in normal and expected outcomes. They know to watch for red flags to ensure they can guide you further if you have come outside the normal, expected process. Their job is to provide physical and emotional support, encouraging you to ask questions of your caregivers to make sure you’re well informed about what occurs. They have resources and guidelines to reassure you that you’re indeed in the realm of normal, and if things deviate from normal, they can point you in the direction of more resources. Clinical management Lastly, we have the clinical management professionals. These are the folks responsible for the clinical and medical bits of the scenario. They look at the facts and figures, big picture, and red flags to rule in or out the things that are not in the normal and expected category and then make management plans from there. They have the clinical experience of things that fall outside normal and how to manage them. Working together All of these people have a place in the realm of support and caregiving; what’s important is they know their role and responsibility and respect the others’. Where it becomes problematic is when the client receives something different from what she expected to receive. Sometimes, this occurs because the roles of each provider isn’t clear to her, and she might conclude that one person isn’t performing a role properly. Let’s look at how this might apply to IBCLCs specifically. In our example, a mother assumes that a breastfeeding educator* is an IBCLC. She notices that despite consulting with the helper, her breastfeeding issue remains unresolved. She decides to seek more help through a La Leche League leader, who determines that the issue is outside her scope and recommends an IBCLC. The mother insists that she already saw an IBCLC, but received no help. *this person could also be staff at a breastfeeding clinic or nurse who comes to her home This example is typical, and it hurts all support people. The educator gets a bad rep because she didn’t help. The LLL leader is helpless because the needs were outside her scope. The IBCLC profession gets a bad rep because the client misunderstood the different roles and expectations. Clients need to know clearly what their expectations are and who can best meet those expectations based on role, scope, and experience. I want to be asked and welcome being asked these questions! I want you to go and look at the IBLCE website to see what IBCLC's are all about and verify I am indeed and IBCLC and see what scope and standards are laid in place for my profession. I welcome the same questions about being a doula! I would love to see a blog about midwives and how they are different from doulas and childbirth educators (wink, wink, nudge, nudge midwives). All breastfeeding and lactation professionals have a responsibility to work together to ensure mothers have accurate information, so they can receive the support and encouragement they need as efficiently and as quickly as possible. 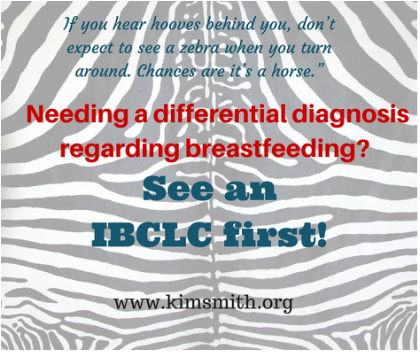 Do you know what can mimic a tongue tie? Terrible breastfeeding technique can. The number one cause of many breastfeeding concerns or issues is positioning and latch. A good latch is vital to milk transfer. Good supply is dependent on milk transfer. Weight gain, pees and poops are dependent on supply. Swing back full circle to latch and latch is dependant on good positioning. This is true in the majority of cases. Add in that good positioning and latch should also make things easy, comfortable and pain free for mother. It should also make things easy, comfortable and effective for baby. When we see concerns with breastfeeding we must start with full maternal and infant assessment. This cannot be skipped. This includes a history on the birth and the start of breastfeeding, how feeding has been going, any know medical issues that contribute to breastfeeding concerns with mom and baby, a feeding assessment including positioning and latch, and structural exams of both mom and baby. Sometimes we have breastfeeding issues and concerns that are easy resolved by refining breastfeeding techniques. It can be that simple. Sometimes you will get breast-feeding technique (position and latch) perfect but there is still lots of trouble. We have pain, we have inadequate transfer, we have low weight, low pees and poops, etc. These are times we need to look further. There can be lots of reasons for this but today I am going to highlight tongue ties. Tongue tie or poor breastfeeding technique? I am all for fixing tongue ties. If they are a problem they are better resolved than to be “pushed on through”. However, I am more if favour of through assessment of breastfeeding & comprehensive follow up if a procedure is deemed warranted which is why I am drawing attention to this point today. Assessment of breastfeeding MUST include watching a feed amongst structurally examination of mothers and babies. And we have to address position and latch. The sooner we do this, the better. Why? Because if we have position and latch causing pain and damage, it is hard to tell if position changes are helping the pain or not. If we have damage and trauma, even a good latch will hurt until that is healed. So, then if look at a baby and see what visually looks like a tongue tie, we start to get blurred lines. The simple presence of a frenum is not a tongue tie. Diagnosing a tongue tie requires more than just looking. It is an assessment of function. Now when we are dealing with breastfeeding infants that function includes transfer of milk, weight gain, position needs, maternal comfort, visual of babies like folds in the lips, blanching of the frenum, blisters in the lips, etc. The people that can assist us in revision of ties are doctors and dentists and I am grateful to have them as part of our team. But, let me ask you how many doctors and dentists are watching feeds? How many would know how to throughly assess a breastfeeding session? How many know what to look for structurally in a mother? And throughly for an infant? Doctors and dentists that we rely on in resolution of breastfeeding concerns by revising tongue ties are typically only looking for a tongue tie as the reason to why you are presenting themselves to them. Their brains are actually wired to look for a possible intervention to try and resolve the issues based upon their skill level, experience and ability to help. Have you heard this quote before? “If you hear hooves behind you, don’t expect to see a zebra when you turn around. Chances are it’s a horse.” This means, first look for the simplest, common explanation to the problem presenting first. Once we have done this, then yes, we should go ahead and look for rarer & more problematic causes. In the medical community this is know as differential diagnosis. How do you know what is causing your breastfeeding issues? The most important key is to telling the difference between the horses and zebras. You cannot do this without a through evaluation, by a skilled practitioner. In the case of breastfeeding, these practitioners are International Board Certified Lactation Consultants. We have to be cautious of not assigning more importance to one element of breastfeeding than another, just because we think it is important or because we think the title of a certain practitioner is important or because that person thinks they are so important. There is another term for this which is “availability heuristic”. It is a bias towards things which you deem as more important because you readily recall it so deem it more probable. So, as someone looking at tongue ties most of the time this is front and centre in their minds. So, it is likely a dentist or doctor would go to tongue ties as a common cause of breastfeeding issues. As IBCLC’s we start at the basics, with the most common explanation of position and latch and move from there. The differential diagnosis mentioned about is what an IBCLC would do. This is why an IBCLC should be a first stop and why I think referrals for revisions of tongue ties should not be done without an IBCLC assessment. I bring this up because I am seeing moms & babies after tongue tie revisions who I didn’t see before. I don't know what the baby looked like before but more importantly what I am seeing a little more frequently than what I would like is bad breastfeeding technique. I cannot help but wonder, if we had just corrected positioning, would that have been enough. Did we have a true tie or did we have symptoms of bad technique that are also symptoms of tongue tie. Looking back at the information presented above about assessments, evaluations, horses and zebras & availability heuristic people you can see where my concern is warranted. Where do you go from here for support in resolving breastfeeding concerns? Be wise in your selection of care providers when you are struggling with breastfeeding. Step #1 should be an assessment with a skilled IBCLC. From there we will make all appropriate referrals to other members of our team that assist with getting breastfeeding back on track. If you are in Regina or in the Regina area, I would be happy to help you navigate your breast-feeding challenges. You can give me a call or easily book online. |
Kim Smith
|


 RSS Feed
RSS Feed
