 I was recently interviewed by Sheila Coles from the Morning Edition on CBC Regina. We were discussing tongue ties, laser revision and new supports coming to Regina. Here is a link for anyone wanting to have a listen http://www.cbc.ca/morningedition/episode/2013/02/14/help-for-tongue-tied-babies/ Some of what was higlighted in the six minute discussion I have summed up below plus expanded a small amount for clarity. The definition of (tongue or lip) tie is restricted mobility as a result of a short and/or tight frenulum. Restricted mobility impacts the function of the tongue. (And the tongue is a key player in breastfeeding). The definition of a tie is a functional one used in conjunction with visual assessment. Using only appearance qualities to make a diagnosis causes professionals to miss some ties but could also lead to over-treatment. Visual assessment alone is not adequate for diagnosis and treatment decisions. The evaluation of function must take precedence over appearance so that over treatment can be avoided. Depending on symptoms will depend on who you may need to help make an assessment. (Lactation consultant, dentist, speech pathologist, chiropractor, osteopath,etc) It can be a interdisciplinary approach from assessment to treatment. 2-12% (and perhaps higher) of the population are said to be affected by ties depending on the population under study and the definition used. There are various grades of ties identified which can impact symptoms, diagnosis and treatment. The current lack of awareness and education are often barriers to assessment & treatment. Like everything in medicine advancements are made. Lasers have now provided us advancement in treatment of oral restrictions with benefits over scissor releases. Scissors bleed, can be messy, cannot always reach all ties efficiently and have more of a one-time chance. Lasers do not bleed, user has more control, practioner can get back further to ensure a deep enough release and can assess as the procedure is being done. Lasers also have anesthetic properties as well as antibacterial properties. Symptoms can be maternal and/or baby: maternal pain, nipple damage, engorgement, mastitis, thrush, low milk supply, weight loss in baby, slow weight gain in baby, failure to thrive babies, reflux, colic, digestion issues, fatigue, slow feeds, difficulty latching, gagging, choking, coughing, breast refusal, shallow latch, chin tremors, clicking noises, fretful Breastfeeding Impact • Inadequate latch that interferes with milk transfer • Insufficient milk intake and inefficient feeding due to inability to maintain and adequate tongue seal • Nipple/breast pain and damage • Compromised normal suck-swallow-breathe patterns • Long feeds • Possible weight gain compromise • Reduced milk supply • Early weaning • Need to supplement Beyond breastfeeding • Bottle-fed baby can also struggle • Babies may have trouble with solid foods (reverse swallowing) • Speech may be affected • Orofacial development (high, narrow palate, orthodontics) • Dental issues • Increased salivation • Airway integrity and apnea Feeding and milk supply concerns can be worked on with the assistance of a Lactation Consultant. There are various tools and management techniques that can be used depending on each unique situation. Tongue mobility is the goal of laser treatment. The secondary results, such as increased milk transfer occur only when treatment restores optimal tongue placement, movement and strength. Function restoral is generally dependent on a team approach to care including dentists, bodyworkers (osteopathy, chiropractic) and lactation consultants. When breastfeeding is the concern the earlier the treatment the better but that is not to say later treatment is not beneficial to other symptoms that may arise. Tongue ties are a controversial and subjective topic currently. The team approach will be growing in Regina soon with a local dentist coming on board to help with treatment.  I asked this question of my Facebook friends earlier this week. What do dentists, midwifes and chiropractors all have in common? I received a wide variety of answers and all were very points. Let us have a look at some of the answers. "You totally dismiss their existence or possible usefulness until it turns out you need one?" This one had the most likes, and for good reason. I don't know what it is like in other places in the world specifically but I know in Saskatchewan what these practitioners are able to do for health and wellness and care is not well understood. Dentists would be the most commonly accepted practitioner of the three but they still are not fully understood as far as their role in things beyond healthy teeth; more to come on that later. Midwives are growing in popularity but again until you need one you probably wouldn't have paid much attention to them and all the benefits they serve in a community and why we so desperately want more of them. I think everyone needs to care about increasing our midwifery numbers and access to them in all communities, not just our currently pregnant moms. And chiropractors; they are a hidden secret in health and wellness. Most commonly known for snapping necks and popping bones back into place even though that is rarely what they do & definitely not what they want to be doing. They really want to help your body be sound structurally since the basis of function comes down to structure. If a structure isn't 100%, it isn't going to function at 100%. The scope and importance of these practitioners cannot go underestimated. "I would guess that they aren't considered necessary to medical care (by the powers that be…)" This was one of my favourite answers, because it some days it really feels that way. There are jokes by doctors that I have heard before such as "What do you call a doctor that failed out of medical school" - "A dentist". Chiropractors and midwives are not easily accepted into western medical practice, either. Both would be considered "alternative" even though as far as practice goes as ancient times. They fell out of medicine for quite some time and in the late 20th century started to become a popular choice again. Having said all this, that wasn't the point I was trying to make. "You refer to them? Or they refer to you?" Next on the list of answers was about my referrals to these allied practitioners & referrals to me. Yes, this happens, both ways. It happens for many different reasons. Depending on where a mother is prenatally or postnatally would depend on the referrals and why, but the point is we can all work closely togther. This leads into the next answer. "All can play a vital role in supporting a healthy breastfeeding relationship, along with lactation consultants create the circle of support for breastfeeding moms and babies with tongue and lip ties." Now, I love this answer. We are getting somewhere on where I was going with the question. I would say that we could have simply said, "all can play a vital role in supporting a healthy breastfeeding relationship, along with lactation consultants create the circle of support for breastfeeding moms and babies" and we could have had I not mentioned the dentists. My reasoning for that is because tongue and lip ties are part of why I posed the original question and because it was in the answer. However, there can be lots of issues aside from tongue and lip ties that a midwife and chiropractor could help with. Add in the tongue and lip ties and, yes, then we need a dentist. But now look at the other person mentioned in this answer and mentioned in the circle; lactation consultants. This was the answer I was looking for. They are all knowledgable professionals, but they are not IBCLC's. Lactation Consultants are at the hub of it all. Some people would actually suggest it isn't really a circle that would be formed but rather think of an IBCLC more as a project coordinator, like a general contractor. The general contractor is a manager. An IBCLC must first assess the breast-feeding relationship. A consult is required to get a better understanding of the breastfeeding dynamics . The IBCLC than can recommend specialized “subcontractors" to perform tasks that are needed to meet the goals of the breast-feeding mother and help resolve some of the challenges. Then the IBCLC as the specialist in breastfeeding can do another consult to fine tune the work of all the “subcontractors”. This is really important as many of the symptoms of tongue and lip ties can be because of many other things. We need someone to assess that all. That needs to be an IBCLC. While the other practitioners have knowledge of breastfeeding and how it all works, they are not specialists in all things lactation. Some of the practitioners are going to assume that moms and babies are working with a lactation consultant and some are going to be a little more forward in making sure that moms and babies are indeed working with an IBCLC. Sometimes we need to plan how and when to fix tongue ties based on what all is happening with mom and baby. An example would be needing to resolve moms milk supply so that after baby has his tongue and lip tie fixed, he is rewarded easily with a good supply. It can be challenging for mom to do this while caring for a baby after the procedure. Another example is oral exercises for baby. You can think about this as rehabilitation. We cannot make a change to a babies physical structures without helping that baby adapt to the changes - again, this comes down to what an IBCLC is going to teach and assist parents and babies with. The IBCLC will further assess for improvements and make recommendations as needed. Keep in mind, these are only two examples of what an IBCLC is going to do. It is really hard to skip over some of the practitioners. Sometimes things will not resolve at all or much more slowly than needed unless we have a solid team trying to resolve the issues at hand. I think it is incredibly important before we go ahead and perform any procedure on any baby, that this idea is well explained, understood & accepted so that ultimate, ideal care is provided to families, especially the baby who needs the most support.  white color that can often been seen after feedings white color that can often been seen after feedings You are a new breastfeeding mother. It has been about ten days and your cracked bleeding nipples aren't healing & you have started to have a burning sensation with deep throbbing pain in your breast. It sometimes lasts for a few minutes, but sometimes hours. The beginning of feeds are terrible and even between feeds you are getting electrical shock like feelings in the breast. If this is you, you are like many other mothers and like many other mothers you may have been told you have thrush. You are given a prescription for nystatin for you and baby. You treat for two weeks and symptoms get mildly better, but it isn't going away. Baby has no symptoms but your pain just won't knock it off. You get Nystatin for a couple more weeks, cut out all sugars, start washing your nipples with grape seed extract and the pain in still persistent. Maybe you have had APNO cream & some Diflucan in there, as well. Still no success. How about I suggest to you that if you have thrown every thrush treatment at your nipples and you're not seeing results, that it isn't really thrush you are trying to treat? Thrush is very commonly diagnosed, rather misdiagnosed. I do not think that it is as common as we are being led to believe it is. I know you are asking me, "if it isn't thrush than what is it?" I would say in more likelihood than not, it is vasospasms. Vado-Whats? What are those? The simple answer is that the blood vessels in the are contracting and becoming smaller in diameter - called vasospasms. This can happen for a variety of reason and for some people it can be very painful and occur in various parts of the body, including the nipple in breastfeeding mothers. There are risk factors for vasospasms including but not limited to :
What are some more symptoms and how would you suspect you have vasospasms?
It is important to seek professional help as soon as possible if this problem is persistent. They can help assess the cause and come up with some remedies for you. They can also explain the use of vitamins, minerals and omega fatty acids (important for healing). There are also prescription medications available, if warranted, and your IBCLC and physician can help accommodate that. You do not need to suffer through the pain or end breastfeeding for this to resolve. If you would like to keep breastfeeding, without pain, book an appointment and we can get you back on track.  Avoid you and baby feeling this way during the holiday season with these simple tips. Avoid you and baby feeling this way during the holiday season with these simple tips. There is a holiday guide for everything - why not have one for breastfeeding? From holiday clothing to preparations to unsolicited family advice, here are some tips for the holidays. Lets start with the easy stuff; wardrobe. If you are going to find yourself breastfeeding at a holiday event, you might find it easier to wear separates, a shirt and skirt, or pants, something that opens from the top down like a zipper or buttons. If you want to be a little more discreet, consider a shawl or scarf you can place along your breast but not have babies face and head covered (many babies don't like that, making it less than discreet). And you can also make your baby an accessory! Get a ring sling or other handy carrier. They can be easy to nurse in, keeps baby close, helps reduce stimulation, less people to handle baby, gives you both hands and provides a comforting spot for baby to sleep while you enjoy festivities. Engorgement, plugged ducts and mastitis are not holiday visitors anyone wants, but the holidays does see a rise in these sometimes easily avoidable issues. The easiest way to prevent these are to nurse often, take breaks from the busy times, preparation, long travel, & shopping. Nurse often and regularly. The bonus is that the oxytocin flow will help keep you relaxed in what can often be a hectic time. If you are hosting a holiday event, don't over plan and over do it. Ask for people to help. Maybe have a potluck dinner, less decorations and don't be afraid to have a quite place that you can sneak away to if you need. Lots of unsolicited advice seems to come up when we get together with our closest family and friends. They all do mean well, so don't be offended. To help them to also not be offended, practice a polite response, such as, “Thank you for your perspective. We have decided that this is best for our family” or “That’s an interesting idea. We might consider that at a later point”. You might not be telling the truth, but thats ok. Simply ignore what you can. Many hands make light work, but those same hands often want to feed the baby. Try to delegate those hands to change diapers, play, or just cuddle baby between feeds. Most of the time, what mothers eat doesn’t cause too much concern for the breastfed baby, but sometimes we indulge beyond moderation and then it can be concerning. Too much chocolate for example can cause fussiness. Peppermint and sage can have a negative effect on supply, so just be cautious with how many candy canes you have. Also, going to note that it is safe to consume some alcohol when breastfeeding, without the need to pump and bump. General rule of thumb - your breastmilk alcohol content is the same as your blood alcohol content. Generally, a drink or two would be 0.02-0.04% - you can see its not enough to worry about. Enjoy your holidays with your precious little ones! May they bring you the magic of the season.  Multiple times today my attention was called to this article posted by Nancy Mohrbacher that brought an idea that tongue and lip ties are an epidemic. I would suggest reading that article first and then looking at my post. Nancy refers to a study just recently released that was trying to prove that the prevalence of tongue tie is higher than the literature suggests of 0.3%-12% of the population. After seeing the responses on social media I am not convinced that that people are looking at the study for themselves and are drawing conclusions from the title alone. Here is the conclusions of the study. "All but one infant (n=199) had an observable or palpable lingual frenulum that was Coryllos type 1 (n=5), type 2 or 3 (n=147), or type 4 (n=47). Although our study was not powered enough to test for any correlation between the cessation of breastfeeding and the type of frenulum, we found no statistical correlation between the Coryllos type of lingual frenulum and the presence of breastfeeding difficulties. CONCLUSIONS: A lingual frenulum is a normal anatomical finding whose insertion point and Coryllos classification are not correlated with breastfeeding difficulties. We suggest that the term "lingual frenulum" should be used for anatomical description and that the term "tongue-tie" be reserved for a lingual frenulum associated with breastfeeding difficulties in newborns." A valid point - A frenum present/observed is not a tie. And there is no correlation between type of "grading" and breastfeeding concerns. In fact, this is why some of us professionals skilled in tethered oral tissues want to eliminate the terms and grading and why I, in my practice, do not use a grading system. (I do have tools and assessments) Moms ask me a lot what class it is - they get this idea from the internet. It is easy to understand a range of 1-4, or anterior or posterior. I will not attempt to grade it because implies one type of restriction is more problematic than another and this might not be the case. It is a little bit harder to comprehend structure and function, central nervous system and how it all plays into feeding. So, I don't blame moms for wanting a simplified tool. The truth is we don't have that. It also seems like grading can validate decisions, to treat or not, based on a grade. "The IBCLC said it is a severe tie and I had to fix it" or "it was just mild so I didn't need to fix it" are examples of what we might hear from most given a grade. Part of the grading is simply for documentation purpose if a revision is done. It is like taking a before picture without the picture. The surgeons preforming frenecomies need a way to document what they see and what they performed. This study looked at infants at days 0-3 and then a follow up at two weeks, by telephone. The lingual frenula of 200 healthy infants were evaluated by visual examination and palpation within the first 3 days after delivery. The frenulum was categorized according to the four Coryllos classifications. Each infant's mother responded, immediately after the examination, to a structured questionnaire on the quality and type of feeding. An additional structured telephone interview with the 179 breastfeeding mothers was conducted 2 weeks later. This raises some questions for me: Is day 0-3 too early to show concerns? Yes, in many cases it is. What we know from the study is 3-4% of the babies had issues they considered to be from ties. But we don't know if all the others were completely asymptomatic after the 3 days or after the two weeks. Are we considering any infants that did have breastfeeding problems to be something other than restricted tissues? This is an unknown. Is breastfeeding established in the first two weeks? No, it is not. What about later onset of issues? So, revisiting the earlier question, we don't know beyond the 3-4% that has issues in the early days if others had issues. There are quite a few symptoms of tongue ties that show up later, like secondary low milk supply, reoccurring mastitis, weight gain concerns, inability to swallow solids foods. There are many symptoms. Too many to list in this blog post. Is two weeks normal term breastfeeding and the optimal goal? No, World Health Organization and the Canadian Paediatric Society recommended breastfeeding for two years. Many undiagnosed tongue tie babies are reported to self wean between 6 & 9 months. Do they intend to follow up longer? This is an unknown. There were 200 assessments done, but only 179 telephone calls made at 2 weeks; what happened with the other 21 dyads? Did they stop breastfeeding (perhaps due to issues)? Again, another unknown. While on the subject of tongue and lip ties on social media in response to this treatment came up, multiple times, and Nancy discusses it in her post as well. We need to be very through in evaluation and looking at the root causes of the problems. We need to seek out the people knowledgeable to do such an evaluation. Depending on where moms live these resources might be abundant or they might be scarce. There is so much to consider when it comes to breastfeeding that we cannot latch on to one specific if things are not going ok. It is often a cascade of things. Sometimes it is partly mom, sometimes partly baby…it is a little like detective work at times. Breastfeeding is fluid and holistic. There are many considerations and options before revision & revisions are not a quick end to the concerns dyads have. One example of what I mean is considering moms anatomy/function when looking at ties. It is a bit like puzzle pieces. A tongue tied baby might not have any issues with a mother with one sort of breast and might with another (think about wet nursing, or even babies who do well on one side and not on another). My clients get presented all kinds of options. We start with what can we do today, right now, to make this better and manageable and tolerable so we can even get to a place of discussing long lasting breastfeeding. Often by the times I see moms I am getting told is "YOU have to fix this or else I QUIT". No pressure. But when a mom is looking quitting in the face, I need to give her some right now options, but also get her as far away as quitting as I can before I leave her because it I don't she is right back at looking quitting in the face. That is why consults are so through and a big plan is made - a right now, a week from now and longer term. So, when I see restricted oral tissues, do I let clients know? Yes! Even when I'm not 100% sure that is the issue, I mention it because moms don't always come back for follow up so I cannot assume that after they try tricks 1, 2 and 3 for a week, and come back so we can reassess. If I don't tell them they might never be told or if the tricks don't work and nothing resolves they are left feeling like it was a failure and give up. If they know that there are things that could work, BUT, if they don't we need to consider the restrictions to having an impact, they are informed. If I see moms early in the process (like day 0-3 when issues might not be noticeable yet) and I can see some red flags I also mention things to just watch for, just as an FYI, because it could become a larger issue. There is also a lot of myths that need to be busted, such as breastfeeding just hurts for the first few weeks, that can be related to ties, so they get overlooked and the problem spirals. Does it mean sometimes moms latch on to that idea and run with it? Yes, sometimes it does. I try to limit that by being very upfront and through in the discussions. I don't get much done in 15 minutes - this is why consults take as much time as they do. History, assessments, evaluations and then discussion takes time. Mentioning it doesn't make me a poor clinician & tongue tie happy (trust me, I dislike them, a lot, and my work would be far easier without them). It does make me through and ensure that my clients are getting a full assessment, not just get a superficial look and a pat on the back that things will get better, that breastfeeding just takes 6-8 weeks to get used to and if they just stick it out it will be worth it. How many times have you heard a mom be told to take some herbs, eat some cookies and drink some beer? That would be fantastic if that is all it took to make breastfeeding easier. But that isn't the truth. Keep in mind, before we had providers who could release ties longer term, we had strategies to deal with breastfeeding concerns. The ability to now release ties doesn't negate or remove these strategies. Why are we not simply just sticking the golden oldies? Because they don't work for everyone, they don't always get people to normal term breastfeeding before they become too overwhelming or exhausting. Because babies are highly adaptable and will compensate and these compensations are not necessarily good for babies and can cause longer term life and health issues. Breastfeeding is linked to so much health wise and it seems like it is acceptable to mention that breastfeeding lowers the rates of commonly known health issues, such as diabetes and asthma, but isn't yet acceptable to say the same things that can cause breastfeeding issues can also cause issues with dental, speech or breathing. I think there are good points to be taken but I think there are gaps in this study and article. Balance needs to be strived for. I would really like to see the documentary Breastmilk vs reading an article about it, however I have not been able to see it yet. So far I have only really seen this article, "Eat It, Drink It, Pump It, Freak Out Over It".
Sounds like there are some extreme scenes, but it is media. Media is made to grab attention. Breastfeeding is not extreme, at least I do not see breastfeeding as extreme or work in extremes with my mothers. The naked breasts in the documentary likely are not intended to grab attention but rather normalize breasts, in a non-sexual manner. The more we see them in a different manner the more comfortable we will be with them as non-sexual objects. I am understanding that the film does not sensationalize breastfeeding. Thank you. You are not a super-star if you breastfeed. You are a woman with a child. It should be an ordinary experience. Again, it should be an ordinary experience. If you live in North America, it likely is not an ordinary experience. In other parts of the world we have toddlers nursing at the playground, entire groups of them. In Canada we don't see that often at all because most of our toddlers didn’t get breastfed must past a few weeks. Toddlers are nursing in Canada, I reassure you of that, but how often does any see this? How often are these mothers comfortable to tell anyone this? And why is it that she is uncomfortable sharing this, when in reality it is recommended in Canada that we breastfeed our children until the age of two and beyond. Shouldn't she be proud she made it to the recommendation? I am also understanding the film to avoid the formula vs breastmilk debate. Again, I say thank you. Not all of the discussions around breastfeeding need to have formula involved. They just do not. Most mother’s who have decided they would like to breastfeed, want to breastfeed. That doesn’t mean it is going to be easy, without struggle, doesn’t need support. That would be silly. It is an aspect of motherhood and motherhood is hard, there are struggles and we need support. We need this regardless of how our babies are fed. If a mother has chosen to breastfeed, it is not a debate. (If a mother makes an informed decision to choose formula, so be it. It is also not a debate.) If a mother choose to breastfeed, she should be encouraged to breastfeed that baby then, and given the supports to do so. Supporting breastfeeding is not to offer formula when it becomes hard. We are culture 3 generations into formula feeding as the ordinary experience, and in culture we look for sameness. This is not a mommy-war, this is how humans function. We look for sameness to find where we fit. Another example is if your mother formula fed you and your are struggling, she doesn't know how to help until she makes your experience more like her own, which is to suggest that you try a bottle. Could this looking for sameness for the reason that the mothers that do breastfeed toddlers are not sharing? In our culture sharing that information does not bring a lot of sameness amongst our community. In small pockets, yes, and those are safer places to share, but our overall culture is still not there. New mothers should not be under pressure to breastfeed. It should be an ordinary experience, with the supports to do so. The weight of the world shall not be on the mother’s shoulders. In fact, I want those shoulders relaxed with arms gently crosses and a baby in those arms. There is a gap in the current health care. You see big decisions about public policy are made at meetings with CEO’s and upper management sort people & doctors looking at research etc. They decide that they are going to have a position that breastfeeding should be recommended and all the reasons why and the hospital and public health offices need to encourage breastfeeding and be on board with the policies. Sounds great. Until you realize the people working directly with the new moms and babies have an even harder job than those making the decisions. They need to actually make it so that moms and babies can breastfeed and they simply do not have the skill set and time to do so. There lies the difference between the 95% that start and the 33% that might still be breastfeeding after several weeks. That weight again is not on the mother’s shoulders. That is society’s responsibilities. The front line workers and their employer's also don't seem to know what they don't know so they share misinformation. Mother’s take that misinformation as truth because these are the people who we trust to do right by us. Or they do not have the time needed for each dyad. Pumping and supplementing or formula supplementation is a faster means to get to the goal, which might be weight gain, mother's to be pain free, etc. Mother's grieve the loss of what they expected. They expected breast-feeding to be easy. Maybe they are succeeding but it is still much harder than they expected. They might not have expected to make a formula choice (which they probably did not make but had to succumb to because the support needed was not there). And so they grieve a loss. We think mother’s feel that as guilt. It is not always guilt mothers feel, it is grief. And it is not always judgement other feel, it is sympathy. I sympathize with the majority of mothers, my clients or not, because it is hard, hard work. And mothers ask for help, identify needs, but those needs often go unmet. They go with mothering let down & disappointed. They feel they failed and are disappointed in themselves. The truth is, they are failed. Mothers do not fail at breastfeeding. They are failed to be able to succeed. You just had your baby 24 hours ago. You feel recovered. Baby is doing well. Breastfeeding could be smoother but the first couple days are hard, right? You are being discharged home. You are a little nervous, but it will all work out, sure it will, or you tell yourself that. “You will all be more comfortable at home”, you are told. True, who gets sleep at the hospital? It’s now night two & baby is up all night long feeding. And crying. And nursing. And crying. All. Night. Long. You don’t know what to do. Your partner doesn’t know what to do. You tell him to grab the can of formula in the cupboard above the fridge. It was the formula that Nestle sent you after you shopped at Thyme Maternity, who so kindly sold your information from their customer loyalty program, to Nestle. You tucked it way back there in that cupboard because you were not going to need it. Now you think you might need it. You don't know how much to give baby, so you just keep giving baby a little bit more until he finally sleeps, maybe 60ml? Or was it 75ml? He must have been starving and you certainly can’t be making any milk if he took that much formula. Surely he would stop drinking when he was full.
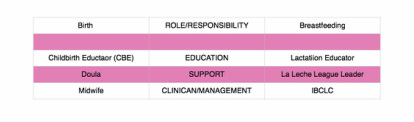
The family in the room beside you at the hospital stayed that night. Mom had horribly sore, cracked and bleeding nipples. Her and baby are also doing good, aside from those nipples. She must not have spent enough time toughening them up. Let her to be a lesson to all of you ladies that are expecting. Get those face clothes out to rub on your nipples when you have a bath or shower. In the morning this mom will get a visit from the lactation consultant on staff. That lactation consultant will be a godsend. Lunch time comes and no lactation comes to see this mom yet. Both her and baby have been given the green light to go home, the LC just needs to come do her part. The LC comes after seeing 6 other moms and babies that were SO happy to see her walk into their rooms. She shares their joy, this LC is finally there to see her. Things will be better now. The LC assesses the mom and baby and her feeding. The LC knows she could help this mom and baby, but there is a problem. She needs more than the 30 mins that this mom and baby still have their room before housekeeping comes to clean up and replace them with a new mom and baby. The LC, whom I adore, can only do so much in this case so she gives this mom as much info as she can, but also recommends getting a pump to keep up supply and letting this mother rest her nipples to help them heal while she works on getting that latch better. Ok, determined, to breastfeed, off they go home. Dad will head out to rent a pump once mom and baby are settled at home. Luckily, a few places have good programs for pump rentals that dads don't need to fret about knowing what to get. Down the street from you, a neighbourhood mom (you haven’t meet her yet, but you soon will at a Mom-and-Tot time) is planning a water birth at home with midwives and her BFF who is a doula. The night comes and she labours peacefully, resting between contractions, with beautiful music soothing her. Her doula whispers affirmations to her and combs her long hair out of her face. Her baby emerges peacefully and they soon move over to her bed. Her baby does a perfect breastcrawl and self attaches. You meet her at Mom-and-tots about three weeks later. Like all the new moms, you weight your babies on the scale there. Your baby is growing, but you have still been continuing to supplement because you just can’t keep up. Her baby seems to not be gaining weight, but he is able to self attach and has a great latch at every feed. She will call her BFF, the doula, and ask what knows about this stuff. Your new friend is reassured that some babies are just slow to gain, and she should just nurse and nurse and nurse, throw her baby in a sling during the day and sleep with baby at night, it’s totally normal for babies to nurse all night long. We all know that all the care providers and mothers in these cases want these babies to be breastfed. We all know that if time allowed more time would be given in hospital to help moms with breastfeeding. The truth is the staff are busy, more moms and babies keep coming in and in order to make room, moms and babies need to be discharged. And we all know breastfeeding is a super natural instinctual event and moms and babies can just do it? Or can they. Was Thyme Maternity sending you the message that breastfeeding is really easy by sending out that Nestle gift bag? The same bag with info that tells you how breastfeeding is best for your baby but doesn’t tell you how to get help if you are struggling? There is no guidance to find a Lactation consultant, even though the International Lactation Consultant Association makes it really easy to find someone near you with their Find a Lactation Consultant link. I have provided that link for future reference. Find a Lactation Consultant Perhaps the hospital could have thought one step ahead and provided you with a local list of people to help, be it La Leche League, that is a volunteer peer-to-peer support group that does phone helping and group meetings, a list of breastfeeding clinics in town, or a list of lactation consultants in private practice that can see you in your home when works for you. The hospital has to be aware that they have time constraints. They also have to be aware that breast-feeding is sometimes challenging for some moms. They also must be aware that if things are not going well that there are resources they can provide to help ensure you are aware of your options, if you so choose to seek further help. Even when things look great in hospital, things can change in the early weeks. Knowing where to get help is important. They can help bridge that gap. Those resources certainly would have helped the mom in the room beside you, too. Or when her husband stopped to get a pump, the pump rental depot could have had a list of people available to give you some additional help. I am sure that she would appreciate that as pumping can be an overwhelming experience to get started with. Your new mama friend with the baby that isn’t gaining weight, she surely needs to know how to access a lactation consultant, because that is too long to go without gaining weight. That mama and baby need help as soon as they can get it. It is not too late for their breastfeeding relationship. However, they do need some additional supports to get things back on track. Let me be truthfully honest here. There are policies and politics at play keeping all of these mothers from getting the support they need and deserve and that is not right. Most people do not know this, most people may not want to admit to this, and then there are some that are frustrated by this all. We are all on the same page, right? We all want moms and babies that want to breastfeed to successfully to able to do so, yes? Or, no? The answer is, yes, in theory but there are things in the way. In my research, I am finding there are guidelines for when moms can have a consult with the hospital lactation consultants and they are so busy that even with guidelines the don't always have time to meet all the requests, and so sometimes moms are discharged before that consult can happen. I am being told that regional staff are not “allowed” to refer to those of us in private practice. I have been given a variety of answers, so I cannot even tell you if that is true and if it is true, why that is. That rental depot that you rent your pump from? Some of them are wonderful and WILL send you in the right direction. Them, I thank. Not all will, so just know to keep looking for help. If in doubt, choose small community businesses, as they are connected to the community. Thank goodness for the peer-to-peer supports, too. When moms just need a mom to talk to to ask those questions that reassure themselves, they are there. And if they don't have answers for mom or it is beyond their ability, they too, will help you find the people that you need. Think about how nice it would have been to hear that on night two babies will nurse and fuss and nurse and cry and that it will pass. “Milk” is there and the act of suckling helps bring in more milk. The nice thing about peer-to-peer groups; you can attend before baby arrives, to help get yourself ready. Doula’s are also really great to ask and will practice much like the peer-to-peer gals. I added this doula to the story, because occasionally, we will see this scenario; a great friend acts as a doula. Doulas are trained in labour and birth support and basic breast-feeding. Most doulas will also be connected to the community and know how to get moms help. What I want you to know is that there are many players on your team to successful breastfeeding but we all have our “position” to play. We can’t play a game of baseball, if we are all trying to be the only player on the team. There are all kinds of bases on that baseball field. Sometimes you need to build your own team. Occasionally, you are thrown a softball and it’s an easy home run. But sometimes, it quite the curveball and you need more help. Getting that curveball to a home run can be a bit of a challenge when people seem like they are trying to get you “out” rather than letting your run the bases one-by-one. If you want an easier home run, I suggest you do some research on the field you are having or had your baby on and make sure you know their version of the game. Oh, and please, don’t do anything to your nipples to prepare them. That really is not needed. The term lactation consultant or LC has become the title for someone with expert knowledge in breastfeeding. They may work with moms and babies to address breastfeeding issues and concerns. They may also teach classes, assist with establishing breastfeeding, and promote and protect breastfeeding. Origin of the term “Lactation Consultant The term “LC” originated as a short form of “IBCLC” or International Board Certified Lactation Consultant because, as you can see, that term is a mouthful. “LC” is not trademarked and does not hold a professional standard like “IBCLC” does, so one will occasionally find a practicing LC who is not an IBCLC. Consumers (mothers and families) and other professionals (doulas and doctors) need to be aware of this. As well, not all those who work as “lactation consultants” in health centres or breastfeeding support centres are IBCLCs. Some employers encourage employees to pursue the credential but don’t mandate it for employment. Many times, nurses with some breastfeeding education fill these jobs. Why is this IBC part so important? The International Board of Lactation Consultant Examiners (IBCLE) awards the title of International Board Certified Lactation Consultant to only the candidates who meet the comprehensive pathway and pass an international exam. This allows IBLCE to establish the highest standards in lactation and breastfeeding care worldwide and to certify only the individuals who meet these standards. Breastfeeding alphabet soup I’d like to explain some of the breastfeeding alphabet soup by using the birthing support alphabet soup, as people seem to relate to that. All the roles are important, but they provide their own distinct scope, responsibilities, and abilities. They can all work together to provide comprehensive support.
Primary roles of caregivers As you can see, I’ve broken this down into three primary roles. 1. Education 2. Support 3. Clinical management Education Educators teach you about the normal and expected processes of childbirth and breastfeeding. They typically call themselves childbirth educators and lactation educators. They teach the normal process of birth and what you can expect when having a baby, as well as encourage and promote breastfeeding. This information helps you make decisions, helps you know if you are on track, gives you references for getting the birth and breastfeeding relationships you want, and helps answer your questions. Educators typically teach community classes in group settings. Support Support people are typically those who have additional training in supporting mother, baby, and family during crucial times: birth and breastfeeding. They’re typically doulas and La Leche League (LLL) leaders. Doulas are usually paid professionals, and LLL is a mother-to-mother peer support group. These roles offer the encouragement and motivation you need to get through the processes of birth and breastfeeding. They’re well versed in normal and expected outcomes. They know to watch for red flags to ensure they can guide you further if you have come outside the normal, expected process. Their job is to provide physical and emotional support, encouraging you to ask questions of your caregivers to make sure you’re well informed about what occurs. They have resources and guidelines to reassure you that you’re indeed in the realm of normal, and if things deviate from normal, they can point you in the direction of more resources. Clinical management Lastly, we have the clinical management professionals. These are the folks responsible for the clinical and medical bits of the scenario. They look at the facts and figures, big picture, and red flags to rule in or out the things that are not in the normal and expected category and making a plan from there. They have the clinical experience of things that fall outside normal and how to manage them. Working together All of these people have a place in the realm of support and caregiving; what’s important is they know their role and responsibility and respect the others’. Where it becomes problematic is when the client receives something different from what she expected. Sometimes, this occurs because the roles of each provider isn’t clear to her, and she might conclude that one person isn’t performing a role properly. Let’s look at how this might apply to IBCLCs specifically. In our example, a mother assumes that a lactation educator* is an IBCLC. She notices that despite consulting with the LE, her breastfeeding issue remains unresolved. She decides to seek more help through a La Leche League leader, who determines that the issue is outside her scope and recommends an IBCLC. The mother insists that she already saw an IBCLC, but received no help. *this person could also be staff at a breastfeeding clinic or nurse who comes to her home This example is typical, and it hurts all support people. The educator gets a bad rep because she didn’t help. The LLL leader is helpless because the needs were outside her scope. The IBCLC profession gets a bad rep because the client misunderstood the different roles and expectations. Moms need to know clearly what their expectations are and who can best meet those expectations based on role, scope, and experience. All breastfeeding and lactation professionals have a responsibility to work together to ensure mothers have accurate information, so they can receive the support and encouragement they need as efficiently and as quickly as possible. In 2012, Finish researchers published a study in the Journal of Clinical Nursing reviewing past studies that had “focused on breastfeeding, breastfeeding support interventions, and education of healthy mothers and infants”.
The researchers combed through 34 studies published between 2000 and 2008 that were focused in Europe, North America, Australia, and New Zealand. At the time they began the study, the researchers pointed out that peer breastfeeding support was rising in popularity, particularly in the UK. Even so, very little research had been done up to that point on peer support, its cost effectiveness, and its impact on breastfeeding rates. Researchers outlined 4 elements that are necessary for peer support interventions to be effective: 1. Well-planned peer education Mothers were generally dissatisfied with the support of their peers if they had received no training. 2. Continuance of support from pregnancy to the postpartum period If new mothers receive no support during pregnancy or at the hospital, any postnatal support would likely be ineffective. 3. Working together with professionals Professional support is critical while the mother is at the hospital and if she experiences serious difficulties while breastfeeding. On the other hand, peer support can better offer advice related to breastfeeding and everyday life. 4. Variety of means to give support This includes such things as individual support, support groups, educational classes at the hospital, hospital-based breastfeeding drop-in centres, pictures, and breast pump loans. The most important requirement for ensuring a successful breastfeeding experience is that the mother feels supported and empowered. Because support must happen over a period of several months, having a variety of trained support persons is integral. It’s unreasonable to expect that a friend, mother, or even a doctor will be able to provide continual support for such a long period. Having a team—no matter how loosely based—can help spread out the burden of supporting a struggling mother. In addition, hiring a lactation consultant can be an ideal combination of peer and professional support. Lactation consultants are educated and trained; they are available for prenatal, natal, and postnatal support in a comfortable and approachable manner; they work with professionals, and they have access to a variety of support methods. Contact me if you’d like to know how I can provide the best support you can receive. |
Kim Smith
|
 RSS Feed
RSS Feed
