 The landscape of breastfeeding discussions has changed. I have been in breastfeeding conversations now, actively, for 12 years. The conversations I am having now do not resemble the conversations I have had in the past. I cringe now when I think about many of those conversations, knowing what I know now. What is that saying? When we know better, we do better…YES, yes we do. One of the primary changes to the conversation is that we no longer can look solely at what is happening with the mother of the breastfeeding dyads, but we are looking at the baby also. I don’t mean positioning. I don’t mean skin-to-skin. I don’t mean early and often feeding. I mean, just as in how we look at a mothers ability to produce milk, we need to look at the babies ability to extract that milk. We know production of milk is primarily about supply and demand. Demand needs to be present first; this is the baby. Expulsion of the placenta stimulates the start of milk production & then the baby needs to drive it from there. If we are seeing something not working as expected, we need to assess both mother and baby. Often what appears as not working is “mom hasn't started to produce, her milk is not in yet, she just can’t produce milk or she cannot produce enough”. However, we then also say, and I am sure you have heard this, that very few women truly do not produce milk or produce lower amounts of milk. We use completely contradicting statements, loosely, but they are taken as hard, fast truths. Or we will say, “No, no, you are making enough for your baby. Of course, you are making perfect milk for your baby. Your body knows what your baby needs. Some babies are just slender. That is how breastfeed babies are. They feed all the time. They are slender. Babies on formula weigh more. Don't worry about it. Just keep feeding," Or have you heard about the mothers being told their breastmilk is made of water. They just don’t make “cream” like their friends. How confusing! When the new growth charts came out, we expected to prove some of these theories .The new charts were based on breastfed babies, internationally, in favourable living environments. There is lots of history to read on the development of the WHO growth charts. In short, people expected to see breastfed babies being slender and slower gaining and waited to be able to say, “we, told you so”. Well, the laugh was on us. The new charts show that under favourable environments and feeding conditions, breastfed babies do weigh more than their formula fed counterparts and on the new charts breastfeeding concerns show up even sooner than previously. For example, it is common at a 4 month check up to see a baby on the old chart to not be gaining on the curve anymore. Now, with the new growth charts, that same baby would show up with less than ideal growth earlier, perhaps at 3 or 4 weeks. Growth failure was being seen as a normal negative deviation and being missed! It appeared almost as if advocates of breastfeeding were trying to downplay growth failure, because they so truly believed breastfeeding is the way to feed an infant and didn’t want to admit when it wasn’t working. I was fascinated by the charts and wanted to know why the data spread that way. (That could be my former career as a Medical Laboratory Technologist shining through). About the same time I started looking at breast-feeding failure with my new set of lenses; the lenses that looked at mom and baby, not just a mother seemingly making too little milk, with pain or maybe without pain, with a screaming baby or maybe a sleepy baby, maybe a baby gaining weight but seemingly hungry all the time, maybe a baby with slow weight but seemingly content. I wanted to know more about all the babies & was learning more about babies. (What you seek you shall receive) I was introduced to the idea that babies cannot always function at the breast well, and therefore, the demand is not put on the mothers supply. Without demand, there is no supply! But can’t a mother just offer the breast more, get into bed for 24 hours for a breast-feeding vacation, do skin-to-skin, put baby in a wrap and walk and feed as baby needs and get that supply up? That is exactly what I was taught. Mom just needed to try harder and get supply up, drink more water, rest, take some fenugreek, drink lactation tea and eat lactation cookies. But, you know what? That wasn’t always working. Not with the cases I was seeing. If the baby cannot function fully at the breast no amount of time at the breast is going to drive supply. At the same time, we also learnt the breast doesn’t function like we thought it did. The new science tells us we make more milk by emptying the breast more, NOT by letting it get full and empty every 4 hours. Hold on, what? But babies don’t like when the breast isn't full, they scream and protest or fall asleep. They are happy when it is full, let-downs come easy and milk leaks into their mouths. We now understand this all as a compensation for babies inability to function and realize that this routine of feeding can, in fact, cause (secondary) low milk supply down the weeks of feeding. If we address the babies issues, we can have proper feeding, proper demand and proper long term supply. We are starting to make progress with this and changing the idea of low supply.
What i am not seeing is a change is how we see the idea of oversupply or overactive let down. If the idea of low supply is often being perceived incorrectly should we not consider the idea of overactive let down or oversupply isn't a true phenomena either? Could oversupply also point back to the baby? Is this another function consideration? I certainly think so. I would like to ask that we consider the let down and supply as normal flow, but, too fast for that particular infant. The infant, for varying reasons (and an assessment would be needed to determine the reason) is having a hard time controlling the flow of the milk. They choke, cough, sputter, leak milk, etc. They might have fast feeds, gain well and seem to adapt to this "overactive let down". As time goes on, supply decreases (we respond saying milk supply is now regulated as nothing was wrong anyway) and soon, the same mom with overactive let down, is saying she has low supply. WHY? Because the baby could not feed correctly from the beginning. They had difficulty at the breast, relied on that fast letdown and now without correct feeding behaviours, just like the low supply moms I talk about above, the demand is not there and so the supply goes down. Something else we now know, that we used to say the opposite of, is that a hungry baby will cry and a content baby cannot be hungry, Regardless of weight gain plateauing on the curve, being slow gaining, so long as baby seemed content, no one worried. What we know how is that as milk supply goes down, appetite of the baby goes down. That appetite is the demand we need! So without the demand, we again will have no supply. This is quite a different tale than has been told in history! Let's keep chatting! If you think you need some hep navigating your breast-feeding I am happy to book a time to see you and your little one. Yes, I am a doula and many doulas offer placenta encapsulating as an additional service. I am not one of those doulas. I am a doula that is happy to refer that job out. Why? There are so many more evidence based things I can do to help new mothers that relate to most of the reasons why they are considering placenta encapsulating. There is simply not enough evidence for me to feel that this is how I would like to spend my time instead of doing the other things I can be doing for clients.  One of the primary reasons women consider encapsulating their placentas is anecdotal information that it can aid in appropriate milk supply. As an IBCLC, of course, I think milk supply is very significant. One of the driving factors of good production is good breastfeeding, early and often. This helps lay the foundation for the days and weeks to come. Breastfeeding, in fact, is one of the reasons I became a doula. We know that better birth experiences also aid in better breastfeeding. I wanted to support as many families as i could through the whole experience, rather than coming in after the birth and trying to catch up. Being there right away at birth and returning within 18-24 hours to see how things are progressing really helps get things off to a good start. Early identification of any potential roadblocks and removing them as soon as possible can make a big improvement to how breast-feeding starts off. There are so many reasons for milk supply being low. If as an IBCLC, we identify a supply issue and a suspect cause, knowing the mechanisms of some of the remedies available helps us know what to recommend to help resolve the issue. Ee do not yet know the mechanism of how placentas work to assist in lactation, if they even do. If we identify a supply risk, there are many more evidence based recommendations that can be made that we know with much more certainty should help the situation.
I will also state that I and other IBCLC colleagues have witnessed mothers with supply issues that resolve after they stop taking placenta capsules. Again, this speaks to us not knowing the mechanisms behind how a placenta might aid or impact lactation. In the end, my skill set as an IBCLC is of much more value than the time I would spend processing a placenta, in my opinion. I do also have some personal hesitations that I wish for people to consider. I am not saying that they need to decide not to encapsulate after the considerations but just that they consider the points. When we discuss postpartum mood imbalances & disorders we need to look at a larger picture than just a placenta. We see many mothers of multiples who state they did not consume their placenta after baby #1 but did after baby #2 and felt better emotionally than the first time. However, did they review the other differences? Baby #1 we often know little to nothing about what the experience of mothering will really be like, we go at it alone, we are not very confident in what we already know and we hesitate to seek out much information. Often baby #1 was a longer labour and longer pushing stage. Going from no baby to a baby, no sleep, constant physical and emotional demands from the infant, plus ones own recovery can be overwhelming. Baby #2, labour might be drastically different, maybe this time more supported, a shorter labour, easier pushing, the lack of sleep one gets with a newborn in the house is not as much as a surprise and there is much more understanding of normal newborn behaviours. Maybe the second time she had a doula, the same lady who encapsulated the placenta for her, and also provided postpartum supports, like helping with baby care so she could nap or helped with dishes and laundry so mom can rest, put up her feet and just focus on breastfeeding. Having some healthy meals with nutritional elements similar to a placenta might be a more regular occurrence the second time. Speaking of nutrients; sometimes it is said that mammals consume their own placentas, so why wouldn’t humans? Some theories are that mammals do it for safety; that in the wild the smell of afterbirth would draw predators near and the mother & the newly born were vulnerable and at risk, so for safety, the mother would quickly consume the placenta. There are also some theories that a mother would be hungry and in the wild food is scarce. Their own placenta vs nothing was the best they could get so it could be considered a last resort for a nutritional deficient animal. We no longer live in the wild and food scarcity is not as prevalent. In this day and age, most humans don’t look at their placenta and see their next meal or have a desire to consume it. Even in the wild, they consume it mostly in one sitting and not small amounts over days and weeks like the placenta encapsulation community recommends now. Even with diminished nutrition in food sources, we can purchase vitamins and foods enhanced with vitamins, which could provide the same effects. There is a study I am aware of that is not yet completed and it does show that the mothers consuming their placentas do have higher hemoglobins at 6 weeks postpartum. However, it has also been commented that there is a chance that the families that have the available monetary funds to pay for placenta encapsulation services, also have the monetary resources to purchases better quality and quantity of foods. The cost of the placenta encapsulations has not been covered for the study. It is a control that needs to be considered. As a former Medical Laboratory Technologist who worked in manufacturing of blood and blood products, I also worry about an appropriate environment to encapsulate and I do have concerns about infection control. I know that might be over-reactive but as someone who had to do quality control, sterility checks and saw the process of recalls, I think safety and specifications are important. I mean, after all, the placenta might be contaminated with poop. Even a small amount of bacteria can cause a big tummy ache. I say that more tongue in cheek than anything, but it is a thought. There is equipment needed to encapsulate and I am just not 100% that the risk of cross contamination is not there. Now, I am not an encapsulator and maybe there are steps in place to account for that risk. I am unsure about that. I am just saying, for me, it is something to think about. In the lab, in food processing, in other areas where contamination is a risk, sterility checks and quality control is what keeps stuff “clean and safe” and where recalls start, if they are needed. Just because you made the organ does not mean it cannot hurt you if bacteria is at play. After all that, we do know that placebo effect can be strong and powerful. I am happy to accept placebo effect if you are and I am happy to refer you to a local placenta encapsulator if your desire is to encapsulate your placenta. Are you looking for a doula? Did you pull up the list of interview questions Was the first one "What is your birth philosophy?" Let me answer that for you. MY PHILOSOPHY Doulas have ideas about birth philosophy, but those should be reserved for their own births. As an experienced doula my philosophy has changed and it ebbs and flows with each birth. My job as a doula is to support your birth, your wishes and desires. That looks different for every client. Some overlap and that’s ok, but each birth is as unique as you are.  I want you to be less concerned with my own birth philosophy and more concerned with how I connect with you, how I identify your needs and how I plan to equip you to meet those needs or how I can help meet those needs. WHAT IS YOUR PHILOSOPHY? I have a system in place to get to the heart of your birth experience. It is not an automated system, because you are as human as I am, but it is a system that is fluid. It helps you and I understand your personality style and now that affects your birth, as well as understanding how you make medical decisions. Yes, we all differ in that, too! It is a way to share and connect with your partner about each others wishes in a unique, fun way. I want to know about YOU. What I did in my own births should have no bearing on your births. What is YOUR birth philosophy? If you would like to tell me about what is important to you at the birth of your baby & get help with learning how to meet your goals, lets get together and chat!  Yes, I am a lactation consultant and yes, I am telling you that you can, and sometimes should, use a bottle to supplement your baby. The trick is knowing when that is appropriate, knowing what the feeding issues are that require supplementing and a plan to addressing the feeding issues. Bottom line is babies need to be fed. That is the first rule. If a baby is struggling to feed at the breast, we have to feed them in an alternative manner. Believe it or not, hungry babies are not demanding babies. This is why we weigh babies and ask about pees and poops and mood, etc. We cannot trust a sleeping baby is a happy baby or that a hungry baby will cry. Babies that are failing to thrive are often the seemingly the most content, “easy”, passive babies. A quiet baby often concerns me more than the one with strong lungs demanding more attention. Supplementing in the first few hours and maybe even the first couple days can be done easily with a syringe, finger feeding or a cup. But as babies get older and supplementation either needs to be introduced or continued, the volume of breastmilk needed goes from a few drops to a couple ounces at each feed, and many parents need something faster, less finicky and overall more convenient to use. That sounds like a bottle to me! I know, I know. We shouldn't introduce bottles and nipples or formula for 4-6 weeks while we get breastfeeding established, right? ALL the books say so! So I mustn’t have a clue what I am talking about. Yes, those “rules” are sufficient if there are no feeding concerns. Rules are made to be broken and when we have feeding issues and concerns, we need to break some rules to get resolution. In fact, we are not really breaking any rules, since those rules are written for the average breastfeed baby, with no feeding issues. The babies I am talking about are babies with feeding issues, concerns about intake and weight and have a need for supplementation. You might be saying, OK, but what about a Supplementing Nursing System (SNS). An SNS might be an option, but again most parents report they are finicky and hard to learn about. The other concerns are they are expensive, hard to buy locally. I would also add in that with a plan to resolve feeding issues, supplementing would be short term and a bottle wouldn’t be used long, so easier to access and cheaper to buy. The SNS also wont help supply if baby is not feeding effectively. A SNS is a great option for long term supplementation needs that some mothers experience with conditions like Insufficient Glandular Tissue. This is a less common breastfeeding issue than what I am discussing in this post. The sorts of breast-feeding issues I am talking about are babies with no, slow or low weight gain, tongue ties, birth injuries, post birth feeding delays, secondary low milk supply and sometimes a combination of these concerns. What is vital to understand is that a baby that is slowing gaining, holding weight but not gaining or is losing weight cannot effectively feed themselves. They will spend hours at the breast. Mothers report feeding for 5-6 hours straight & cannot understand how with all the feeding babies are doing they are now gaining adequately. The answer is to this plainly and body simple. They are not feeding, they are pacifying themselves. With this their appetite delays or diminishes and they never demand to be feed. They are content to nurse when placed at the breast, they will swallow with let downs or breast compressions but they are unable to stimulate more let downs and cannot extract milk from the breast. As this happens the mothers supply will decrease and the cycle gets vicious. With a decrease in supply, there is a decrease in let downs that just simply occur and babies get even less milk. The feeding becomes all mother driven. By giving these babies bottles (breastmilk or formula depending on the situation) , getting the volume they need into their bodies, their weight increases, their appetite increases, their desire to feed increases and then moms supply increases in response to the baby. I would say any of these situations should have a skilled lactation consultant involved to know the amount of supplement needed, now often and for how long. Depending on the reason for the initial feeding, there might need to be more of a plan in place to then decrease the amount of bottle feeding, but that also needs to be addressed with skilled lactation care. If the initial reason is left unresolved then taking away the bottles will just result in more concerns. Bottom line is, sometimes bottles will be what saves breastfeeding. Yes, bottles are an intervention, but intervention doesn’t have to be a bad word.  In a day of instant connectedness it is really easy to want to announce something you have been working on for 9 months…YOUR baby! What an exciting time for you. And you know you have a whole lot of friends and family waiting to hear the news. GUESS WHAT? It does not matter if they hear that news 5 minutes after the birth, 5 hours after the birth or even 5 days after the birth, if that is how long you choose. I do encourage you to wait longer than 5 minutes though. Those first few hours are oh, so precious. And they will not ever happen again. You cannot get them back & do it differently. You need to live in the moment at this time. There is no past and no future. There is just "right now". I promise you, you will feel like the world stopped as you welcome your baby. Embrace that. Be selfish about it. This is your baby. In that first hour or two after birth, your baby wants to re-connect with you. That baby has been only connected to you for 9 months. Now, it needs to re-connect in a new way. Be mindful in this moment. Stay focused on your baby. You will have enough people in the birth room, you don't need to get on the phone, or Instagram or Facebook, or FaceTime or SnapChat. Limit the distractions. Even sending a quick text with the announcement creates ripples you might not think of…like unexpected visitors at the hospital without your knowledge. I have seen it a few times now that a text goes out, parents get busy & don't respond to returned texts (duh, they just had a baby, of course they are busy) of “when can we come to the hospital” and as we walk out of Labour & Birth, visitors are waiting in the waiting room and simply follow along to the Mother Baby Unit. New parents don't want to say “get out” & they shouldn't have to. So they don’t, but they do later confide in me they wished they had had more time before visitors arrived. When we lose our focus, we lose momentum. And so do babies. In those first few hours, they are trying to adapt and make a little sense of their world. It’s hard work for them to learn to feed and get to know mommy a new way & meet daddy on the outside world, figure out that the hospital staff are different people and keep going. It is even harder to do when they are being stroked, picked up, passed around, kissed by everyone and all the chatter and squeals of excitement. Babies need to have time to learn now this all works. Teach them gently. Again, be selfish about it. Allow yourself to transition to mothering and fathering. And then decide when and how to tell everyone. You will be much more level headed and able to answer questions about when you want visitors and can handle the commotion and are ready to be vulnerable to people. This is one moment in your life that you will feel the most vulnerable. Protect yourself, too! P.S. Do yourself a favour and don't send out "I am in labour texts"…your phone will go nuts! And people might decide to camp out in the hospital waiting room once you stop responding. I promise, in labour, you no longer give a damn about your phone!  …stop ignoring the bigger issues when it comes to breastfeeding and babies. It is no secret I love essential oils. I really, really do. (I am a very committed doTERRA user) It is also no secret that I love helping moms breastfeed, to the point of making a living doing so. But, there are only a few people who know how much I dislike the use of essential oils for breastfeeding related concerns - like low milk supply or fussy, gassy, colicky babies. Surprisingly, it is not because I don’t think essential oils will help with those things. It is because there is almost always something more that needs addressing under those symptoms. I am a huge advocate for alternative wellness. I think there are so many options out there for people to maintain optimal wellness and I am accepting of all sorts of options. However, I am also an advocate of knowing what it is one is dealing with when it comes to being off track from ideal wellness and I am especially passionate about this when it comes to babies. The truth is, there are very few people who understand lactation and so even when a mother sees a doctor who tells the mother she has “low milk” or “baby needs to be supplemented” they are not answering a very important question. That question is WHY? Why is the supply low? Why is baby not gaining as we expect? Breast-feeding is the biological expected way to feed an infant, but sometimes it isn’t as easy as one would expect for such a natural act. There are so many reasons why mothers and babies struggle with breast-feeding. We could make a large laundry list of reasons although the little list would be not enough milk or it is/was too painful - sometimes both. Moms should know that they can look into it further & babies deserve that, too! There are many reasons for complaints of low supply, weight gain issues, pain, and so many symptoms to tell us that breast-feeding is not working as smooth as it could be, or that baby is not feeling as well as a new baby should. I am thinking of things like sore nipples, low milk supply, low or no weight gain, a baby that is not seemingly full and happy, colicky, gassy, not pooping (YES, babies NEED to poop….disregard all the old opinions that breasted babies don’t poop frequently), not sleeping like a newborn (I don't mean to say babes sleep 8-12 hours a night and that is what you should be seeing. I am meaning naps and being able to be put down for little stints at a time vs a baby that is never settled & always falls asleep at the breast but startles as soon as he is set down). These are all symptoms of a mother and baby that could use some help with breastfeeding. And yes, oils could help alleviate some of the stress and reduce the symptoms. I won’t say that they won’t help. But wouldn’t it be nice to figure out WHY this is occurring so that one doesn’t run into more troubles down the road? Using oils to help alleviate symptoms a little bit can make things seem better for a short time but in the long run can delay mothers and babies getting help they need and ultimately can end the breast-feeding relationship sooner than baby would like, and you better believe it, even sooner than a mother may like. When I work with moms and babies that are struggling to keep breastfeeding going and I do a history intake the dyads, so many times there are red flags in the early days. Most moms are told these are “normal” and not to worry, so they do not. We need to start paying attention to the first few days and weeks to make sure mothers are able to meet their goals of months and years of breastfeeding. Don’t just hand out some samples of myrrh for those sore nipples, or some fennel for that low supply or upset baby tummy. Get moms some samples in hand and do mom a favour and give her a recommendation for a solid lactation consultant (IBCLC) in their area to make sure that 1) the oils would be the right oil for what is going on and 2) help mom figure out why things are not working as smooth as they should be. In the end things are cause breast-feeding issues can also be affecting other areas of life for mothers and babies. Breastfeeding issues are not isolated to breastfeeding.  Should you make a birth plan? When I first was introduced to birth plans, I thought, well of course you need a plan. How else will someone get what they want for their birth and how else will everyone else know what they want if it is not planned? In my doula practice, I was working with clients and their birth plans, if they had one all, mostly looked the same. Almost 100% of them were geared to an unmedicated, vaginal birth, little to no interventions, low lighting, music, immediate skin-to-skin, delayed cord clamping and the baby doing the breast crawl. Everyone wanted the same thing. What they had in their plan sounded great & is completely obtainable. Can you feel the however coming on? However… Many mothers use the birth plan template that comes with the specific childbirth education class or system they are studying or they pull one off the internet. The templates usually look like check boxes and people check what they want off the list or they are very specific for one way of birth and do not show all the option available. This limits the choices and options women would have, before they even start labour. In reality, the experiences clients were having were not turning out to look like the birth plans they had. There are many different reasons as to why that is, almost as many reasons as there were births. Some people were a-ok with the deviations from their birth plans and others very much were not. I was curious about they why behind these feelings and was determined to figure out the differences. I will also mention here, that the people without birth plans had a mix of being very pleased with their birth experiences and others that were not so content with their experience. Just going with the flow of birth and avoiding a birth plan also wasn't working for the majority of people. I have also seen doulas and childbirth educations encouraging birth preferences. This began in response to the idea that a “birth plan” is too rigid and mothers were feeling like they “failed” their birth if it wasn't in line with the birth plan. There are also concerns that showing up at the hospital with a birth plan is too strong and is being interpreted by the staff as being told how to do their jobs. Birth preferences is a lighter tone and just means that you would prefer a certain way but would be fluid in the desires, if needed. The hope would be that this results in less failure for mothers & appear less aggressive to the staff. I have always thought preferences was too weak, to be honest. I had started to encourage birth visions with birth plans. Imagining what someone would like for their birth and think that desire through often. This came from the idea that “thoughts become things”. Rather than focusing on the things people don’t want and being more negative in tone, that people should focus on the positive aspects of the birth. Ideas like who they see attending the birth, what position they see themselves birthing in, what things do they want to see and hear, what do they imagine themselves and baby doing after birth. This felt a little better and like I could really get an idea of what people wanted to feel at their birth. But these visions were still harder to put down on paper, so it was not much stronger than birth preferences. I preferred this way the most but it sure had room to improve. The Discovery of Your Birth Experience In trying to make peace with birth plans and make them into a workable, viable option, I discovered Your Birth Experience (YBE). I was the first in Canada to start using YBE. Before I started, Missy and I had talked about Canadian relevance. Missy offered me the chance to critique the program and see if I felt it would be a good fit for birth in Canada. I have to admit, I opened it, saw “Birth Plan” and wanted to close it up. Another program based on Birth Plans! This isn't what I wanted. But, I told Missy I would review it all, so I started reading. Page 2, I started to feel curiously optimistic. By the end I was friends with Missy again and knew this would work for my clients. In YBE, we help clients make birth plans, but the birth plan gets built as clients become educated about themselves, about birth & about the choices they have, options available to them and the interventions they may be offered. The building of the birth plan is actually the finished project of the exploration and evolution of learning. It is not a check list of nice sounding ideas. It is used a tool to prepare for the experience. Many of the outcomes of previous experiences made sense as I would work through the YBE content and training. What so many clients were doing was just pulling birth plan templates off the internet or out of a birth book, checking off what sounded nice or what they thought they should pick. What they didn’t do was any learning about how to actually achieve what they checked off and missed creating the actions of that birth plan. If they want an unmedicated, vaginal delivery, do they know what they need to do to make that a reality? Do they have coping techniques planned out? Are they practicing those? If they know they want an epidural, do they know what that really means? Do they know they would then have an IV, have limited movement and usually a catheter? The choices are theirs to make, so long as people know what it all really means and are prepared for what comes with the choices. If people understand and say “yes” to that, then they feel good about the experience. In YBE, we give you want you need to make a birth plan but more importantly, we give you the tools you need to achieve what is in your plan. I emphasize “your” plan, because it is about you and your experience and no one else’s. I invite you to learn more about YBE, schedule a private or group class or join an already scheduled class. 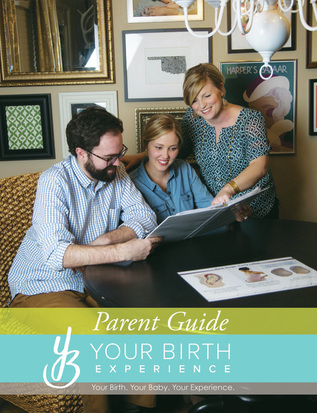 Birth preparation is important! However, you do not need to become a birth expert to give birth. What I mean is, you do not need to commit weeks and weeks and a large number of hours to a prenatal class in order to have a baby. What if I told you could attend a 5 hour childbirth class? Yes, simply FIVE hours. There will be some homework, but I believe you are capable of doing this all on your own time. You will get from the homework what you put into the homework! I am there to help you with the homework, too. Your Birth Experience is designed to connect YOU with all your childbirth options in a unique way. You won’t find a program like this anywhere else. It is comprehensive yet personalized to you. In Your Birth Experience, there is CONNECTION to each expecting family, IDENTIFICATION of their individual needs, resulting in families being EQUIPPED to achieve their unique birth experience. Everyone receives a copy of the YBE parent guide, complete with colouring pages. Yes, colouring pages. Colouring is a great activity in pregnancy & labour. You will learn evidence based information on the process of childbirth and potential interventions. You will envision your ideal birth experience and be provided with the tools that you need to make that happen. Note, that it is YOUR ideal birth experience, not mine, or anyone else’s. You will learn labor comfort measures & relaxation techniques and we will practice them. You will explore and discover your unique personality styles, how you tend to make decisions & how this affects communication.Communication is very important in labour and birth. You will be able to create a birth plan that effectively communicates your desires to your birth team. This helps you create the best environment for you and your birth team for your own unique birth experience. We will also begin our entrance into the world of breastfeeding in this class. I say begin because there is a more in-depth breastfeeding class that is available. I have them broken into separate classes for a couple reasons - to help make more breastfeeding classes accessible to people taking other childbirth classes & your time commitment, you can break up learning sessions. What won’t you find in this class? Videos of women giving birth. You are saying, “What? No videos? Why not?” I can tell you, that as a birthing woman, you will NOT be seeing or feeling birth from the angle or perspective that you will see in the video, so it might not be of any value. Another big reason is most of the support people we bring to classes with us do not want to watch birth, and also, may not be experiencing birth from that angle of perspective either. They are uncomfortable watching videos in a group setting and to be fair and honest, do not digest the content because they are distracted by the discomfort. Birth is a right brained activity, meaning we don't need to see birth to give birth. And another big reason, YouTube is full of birth videos. If you feel birth videos are important to watch, you have hundreds and hundreds available to you. You don't need me to facilitate viewings. We do, however, watch a video about breastfeeding. Breastfeeding is also a right brained activity however does have a left brained component to it, so it is helpful to see breastfeeding when preparing to breastfed. You also will not hear about all the complications of pregnancy and/or birth. This is important for a few reasons. 1) I don't want to scare you. We will talk about fear in the class and how fear inhibits labour. 2) If you do have a unique concern in your pregnancy or birth, that is where your trusted care providers are your best resource, not your childbirth educator. I am a resource for you, for sure, but we do not need to discuss ALL the possible concerns, in order to understand the one or two you might be having. 3) Back to the communication I mentioned earlier in this post. I will help you to be able to communicate with your care provider so that you have all the info about your unique concerns. That is important. 4) There is info in the YBE Parent's Guide about possible complications and interventions, so you do have information. We just do not spend lots of time in the class because it doesn't universally apply to all. I invite you to the next session of this class and am excited to help you prepare for Your Birth Experience. This class can also be done in your own home, one-on-one, if you prefer that option. Simply contact me to set that up!  Do you know what can mimic a tongue tie? Terrible breastfeeding technique can. The number one cause of many breastfeeding concerns or issues is positioning and latch. A good latch is vital to milk transfer. Good supply is dependent on milk transfer. Weight gain, pees and poops are dependent on supply. Swing back full circle to latch and latch is dependant on good positioning. This is true in the majority of cases. Add in that good positioning and latch should also make things easy, comfortable and pain free for mother. It should also make things easy, comfortable and effective for baby. When we see concerns with breastfeeding we must start with full maternal and infant assessment. This cannot be skipped. This includes a history on the birth and the start of breastfeeding, how feeding has been going, any know medical issues that contribute to breastfeeding concerns with mom and baby, a feeding assessment including positioning and latch, and structural exams of both mom and baby. Sometimes we have breastfeeding issues and concerns that are easy resolved by refining breastfeeding techniques. It can be that simple. Sometimes you will get breast-feeding technique (position and latch) perfect but there is still lots of trouble. We have pain, we have inadequate transfer, we have low weight, low pees and poops, etc. These are times we need to look further. There can be lots of reasons for this but today I am going to highlight tongue ties. Tongue tie or poor breastfeeding technique? I am all for fixing tongue ties. If they are a problem they are better resolved than to be “pushed on through”. However, I am more if favour of through assessment of breastfeeding & comprehensive follow up if a procedure is deemed warranted which is why I am drawing attention to this point today. Assessment of breastfeeding MUST include watching a feed amongst structurally examination of mothers and babies. And we have to address position and latch. The sooner we do this, the better. Why? Because if we have position and latch causing pain and damage, it is hard to tell if position changes are helping the pain or not. If we have damage and trauma, even a good latch will hurt until that is healed. So, then if look at a baby and see what visually looks like a tongue tie, we start to get blurred lines. The simple presence of a frenum is not a tongue tie. Diagnosing a tongue tie requires more than just looking. It is an assessment of function. Now when we are dealing with breastfeeding infants that function includes transfer of milk, weight gain, position needs, maternal comfort, visual of babies like folds in the lips, blanching of the frenum, blisters in the lips, etc. The people that can assist us in revision of ties are doctors and dentists and I am grateful to have them as part of our team. But, let me ask you how many doctors and dentists are watching feeds? How many would know how to throughly assess a breastfeeding session? How many know what to look for structurally in a mother? And throughly for an infant? Doctors and dentists that we rely on in resolution of breastfeeding concerns by revising tongue ties are typically only looking for a tongue tie as the reason to why you are presenting themselves to them. Their brains are actually wired to look for a possible intervention to try and resolve the issues based upon their skill level, experience and ability to help. Have you heard this quote before? “If you hear hooves behind you, don’t expect to see a zebra when you turn around. Chances are it’s a horse.” This means, first look for the simplest, common explanation to the problem presenting first. Once we have done this, then yes, we should go ahead and look for rarer & more problematic causes. In the medical community this is know as differential diagnosis. How do you know what is causing your breastfeeding issues? The most important key is to telling the difference between the horses and zebras. You cannot do this without a through evaluation, by a skilled practitioner. In the case of breastfeeding, these practitioners are International Board Certified Lactation Consultants. We have to be cautious of not assigning more importance to one element of breastfeeding than another, just because we think it is important or because we think the title of a certain practitioner is important or because that person thinks they are so important. There is another term for this which is “availability heuristic”. It is a bias towards things which you deem as more important because you readily recall it so deem it more probable. So, as someone looking at tongue ties most of the time this is front and centre in their minds. So, it is likely a dentist or doctor would go to tongue ties as a common cause of breastfeeding issues. As IBCLC’s we start at the basics, with the most common explanation of position and latch and move from there. The differential diagnosis mentioned about is what an IBCLC would do. This is why an IBCLC should be a first stop and why I think referrals for revisions of tongue ties should not be done without an IBCLC assessment. I bring this up because I am seeing moms & babies after tongue tie revisions who I didn’t see before. I don't know what the baby looked like before but more importantly what I am seeing a little more frequently than what I would like is bad breastfeeding technique. I cannot help but wonder, if we had just corrected positioning, would that have been enough. Did we have a true tie or did we have symptoms of bad technique that are also symptoms of tongue tie. Looking back at the information presented above about assessments, evaluations, horses and zebras & availability heuristic people you can see where my concern is warranted. Where do you go from here for support in resolving breastfeeding concerns? Be wise in your selection of care providers when you are struggling with breastfeeding. Step #1 should be an assessment with a skilled IBCLC. From there we will make all appropriate referrals to other members of our team that assist with getting breastfeeding back on track. If you are in Regina or in the Regina area, I would be happy to help you navigate your breast-feeding challenges. You can give me a call or easily book online.  Nipples sore? Sore nipples can be one of the more common breast-feeding challenges. You certainly are not alone in this, however, you don't need to remain sore, or worse yet, in pain. Pain at any point is your bodies way of telling you something is wrong and you need to pay attention to yourself. What causes soreness and pain? Most commonly it is because of trouble with positioning and latch, creating friction, and proceeding them to soreness, cracks, blisters, bleeding and sometimes infections and even lose of skin. What can be done? Here are a few quick ideas. Most importantly, check your position and your comfort. One of my rules is to make sure mom is comfortable first. Ideally, mothers are slightly reclined, arms and shoulders lose and down, and her neck has the ability to be relaxed. With this, mothers can then bring baby to them. You don't want to try to take your breast to baby. Baby can be front-to-front with mom, being supported by mother’s arms, and mother’s arms can be supported with pillows. Use gravity to help baby get on the breast deeper, rather than sitting upright and having gravity pull baby down or away from the breast. If we still have discomfort, we need to check baby’s latch. A good latch is vital to comfort but also to long term duration of breastfeeding. A good latch is key to effective feeding which is essential for adequate milk supply. You might need to ask someone for help with checking the latch. If someone tells you it looks good, but you have pain during or after a feed, you need to ask someone else. If position changes do not help with latching issues and soreness and pain are still prevailing sometimes we need to look farther into reasons and makes plans. Sometimes we can use a nipple shield to help protect the nipple and help baby to latch. It is important to get good help if needing a shield. There are important things to watch for such as fitting, proper placement, adequate milk transfer, babies output and weight gain. This is very important to know and recognize however; nipple shields are a Band-aid solution. They are not an answer, they are simply a tool to help keep the baby breastfeeding, at the breast, rather than quitting breast-feeding or going to pumping and feeding another way. It is a short term tool that needs a bigger plan. Throw away the lanolin! For years we were told Lanolin was fabulous and all new mothers needed it. But the new research shows us, doing nothing is actually more effective than lanolin and in fact lanolin can delay healing, making things even worse for a longer period of time. Mor effectively you can apply breastmilk to the nipple or coconut oil or calendula if you want to try something else. Do not let you nipples be wet and cold at the same time. Again, we were told for years that we should let the nipples air dry. But for mother’s with very sore, damaged nipples, the cool air can cause more harm. It is a good idea to apply heat while the nipple dries. Something like a rice sock or heating pad after baby unlatches, or even when getting out of the shower or bath, can help. This helps bring blood flow to the nipple that previously was restricted. Soreness and pain are not considered normal for breastfeeding at any time or for any length of time. If basic positioning and latch changes do not help, it is worth having someone skilled come and have a look. They can help assess and evaluate what might be happening and help you make a plan to further overcome the struggles. I might hear “I want to be a doula” as often as I hear “I want to be a knitter”. I am both a knitter and a doula in Regina and I think the two acts have quite a bit in common. Some people are just born to doula and some people are just born to knit. Others need to be taught. They will say, “I want to learn to be a doula” or “I want to learn to knit”. Guess what? Depending on where you live, there is relatively easy access to trainings and teaching for both. I have taken both doula training and knitting classes. This is why I think knitting is like doula’ing. Knitting classes are relatively short. They are meant to teach you basics and get you going, some even construct one particular item, like a hat or a shawl. At the end of the class you have learnt some basic knitting steps and completed a simple item. Doula training is also short & teaches you the basics of birth, some coping strategies and some ideas for your clients; mostly with one type of birth in mind, unmedicated vaginal birth. Quite a number of people enrol in doula training but can’t seem to get themselves off the ground and into the role as a doula at birth. They might be able to attend a birth or two of friends or family, maybe an acquaintance. After those initial "hot" leads, it isn't so easy to get much more opportunity or experience. Many struggle getting paid for the work they are doing & the time they are committing to. Lots of people take knitting classes, but never pick up their needles after the initial items made in a group setting are done. Now, I know most people don't learn to knit so they can make a profit, but if they did they are hard pressed to get people to pay them for their time knitting. Both knitters and doulas get stuck here.  You took a class or a training. Now what? What happens if you want to make another knitted item after knitting class? You likely need to read and perform a pattern that is entirely new to you. You need to evaluate if you have the skills to perform that pattern. If you can do it, that is fabulous, off you go knitting. If you don’t have the skills, you have to obtain them somehow. Or alternatively, you have to pass up the project. What happens if a new doula meets a situation she didn’t come across in doula training? She also has to evaluate if she has the skills to navigate the situation. If she does, she moves along supporting the family. If she doesn’t she will need to obtain them. Or refer to someone else. Sometimes neither happens and both the doula and the client are stuck. Potential knitting projects are unlimited, just as much so as the different kinds of births a doula will witness. To be honest, I feel a weekend of training or a few hours of knitting with a skilled instructor is not enough to prepare us for everything we might desire to knit or might see and need to support our client through as a doula. We need to understand our limitations of knitting skills just as much as a limitations to our doula capacity. Doula’ing also gets treated like a hobby, as knitting would be considered. I think there are a few reasons for this. If we were doing doula “right” then we wouldn't be churning over doulas like butter, because sometimes this is how it feels. We see many new doulas trained every year and very few stay practicing year to year, and we lose just as many "old" ones in the next 2-3 years from when they trained. We really have no more doulas now than we did 7 years ago when I trained, we haven't changed anything in the community to enhance birth & increase the desire to have a doula. It is treated like a hobby which does nothing to enhance our professionalism or create a bigger interest in doula to the larger community. There are many reasons why this is, but compare it to knitting again. In order to advance my skill to different projects outside the knitting class I took, I needed more support to continue growing my skills, and I had to seek that out after the class, sometimes in the middle of a project & sometimes before I started a new one. The reality is that many people in my knitting class set the needles down and never returned to knitting after the initial projects because they didn’t know how to get more skills, didn’t know who or where to turn to, or didn’t have the resources (time, money, etc) to do so. How to convert being a doula from a hobby to a business? If people want to move from hobbyist doula to business doula there is also a huge amount of skills needed to be able to this, too. Again, some people come to those skills naturally, some have to learn it and others frankly pay someone to handle business stuff for them. But lots of what we need to do to move from hobbyist to business doula is looking at how we are "doing" doula, what skills we need to improve upon and how to get good client outcomes. Birth is unpredictable - that is the only sure thing about birth. But that doesn’t mean birth just happens to people and they should just roll with what may be. Birth can be a positive experience for everyone. It is time to doula differently. I am up for the challenge to connect to my clients, identify their needs & equip them with the tools they need to meet those needs because Your Birth Experience matters. Just like learning to knit more than basics by advancing my knitting skills and performing the same stitches over and over until I got the beautiful outcome I wanted consistently, I have advanced my doula skills to do similar steps and processes with clients to make sure I understand my clients needs, I am able to perform the necessary steps to meet those needs and consistently get good client outcomes. This isn't to say people and birth are processes and a systems, because I do not believe this is the case, I believe all people are births are unique. Rather what I am saying is that by using systems and processes, I can get to know people and their desires for their unique birth experience. If you would like to chat about your desires for your birth, consider booking a complimentary consult. YOUR BIRTH, YOUR BABY, YOUR EXPERIENCE
Your Birth Experience is designed to connect YOU with all your childbirth options in a unique way. You won’t find a program like this anywhere else. It is comprehensive yet personalized to you. In Your Birth Experience, there is CONNECTION to each expecting family, IDENTIFICATION of their individual needs, resulting in families being EQUIPPED to achieve their unique birth experience. As I am sure you are finding, pregnancy is a busy time, and most of us already lead full busy lives. Trying to get to 6-12 weeks worth of classes can be a challenge, or simply put, undesirable to many people. Some people don't like large classes, don't have the attention span for hours and hours of lectures and videos. Some people like intimate groups where they already know or can get to know other people. I am pleased to offer Your Birth Experience, for all those reasons, and more. I am also happy to offer the program in a variety of formats based on individuals needs and desires. In group classes, set for 2 hours each over the span of 3 classes (can also be offered in a one day format). I also offer, 5 hour private classes, which can be scheduled in one or two sessions. These would take place in your home & can be scheduled when it works best for YOU! All of the options include:
Your Birth Experience Class is $225 & includes the Your Birth Experience Parent Guide. Your Birth Experience Parent Guide is available book to work through on your own. $65 For more information see Your Birth Experience.  Very few days of my previous career stick with me like the one I am about to share. At the time, I didn’t realize to what extent that day would change my opinion and outlook on many things. A couple brought their very ill young infant to the emergency room. I was called down to do blood work which was standard procedure. After having a difficult time drawing the blood I returned to the lab to run the tests & analyze the results, hoping to shed some light on why this infant was so ill. Some of the initial tests gave results that led to further testing. One of these further tests was a “blood smear”, where we smear blood onto a slide and look at it under a microscope. As I was looking at the smear, I started to think that something was wrong with my equipment or my reagents; something was greatly wrong. My blood smear looked like something I had never seen before. I made a new slide and the same thing happened. I changed all the reagents that could be contributing to the bizarre results. each test gave the same outcome. I needed to accept that this was how this child's smear was. This told me why he was so ill. The baby’s treatment continued. Testing continued. My shift ended. I returned the next evening still thinking about this infant and wondering if we had any more answers. I wasn’t prepared for what I heard and couldn’t believe it when I heard it; the infant has passed away, and the cause of death was malnutrition. He had been fed Coffee Mate and water in place of infant formula. I asked myself, as you may be asking yourself, how does this happen? It turns out it happened, because the family became dependent on the food bank for food, including infant formula. When there was a shortage of infant formula, the parents decided to substitute with Coffee Mate and water. Some will say that it was because they were illiterate and didn’t know the difference. Some would say it was because it resembled infant formula. Some will say it’s because a milk-like product equals milk-like product. This experience stays with me, and I reflect on and react to the action of infant formula being distributed at the food bank. Food security is a basic need, and, for an infant, it’s one of the few things they need and they need often. How does formula get to the food bank? Often the samples that are sent to new parents end up there. Women who choose to -and successfully- breastfeed then have these cans and bottles of formula sitting in their homes in dark cupboards, on top of the fridge, and other out of the way places. They know they will never use it, but the idea of letting it go to waste or ending up in the garbage isn’t something they want. They think about all the moms who have less than they do, less support to breastfed and use the food bank - and think that if they take it there, they can help a mom. Moms who need the food bank go there, they say that formula is available, and they take it. That helps the family budget. Formula is expensive and is likely a large part of the financial stress of the family. What’s wrong with that? The samples don’t come consistently and frequently enough to sustain the food bank supply. There will be times when the food bank doesn’t have a supply of formula but the mothers are assuming it will be available so the income gets budgeted to other items. Now, the food bank has no formula, and the family has no money. They still need to feed the baby. In my ideal dream world, the supports these families would receive would be breastfeeding support as well as prenatal and postnatal education. Breastmilk is virtually free. With even suboptimal nutrition, mothers still produce a perfect, free food for their infants. Infants can be sustained for a significant amount of time on just breastmilk.. The recommendation from WHO and CPA is 6 months exclusively and then continued to two years or beyond, with the introduction of solids at around 6 months. In the event of a food crisis, a mother could sustain her infant for the better part of its first year through breastfeeding alone. The support aspect would be important for that to happen. These mothers also need the education. Many of them believe that without an optimal diet, their breastmilk isn’t good for their baby and that formula is better. All mothers want the best for their babies. They need to be taught that they’re what’s best for their babies. They also need to be taught what normal infant behaviour is. If they don’t understand normal infant behaviour , they may feel like they’re starving their baby. Without access to infant formula, they would likely plug along and make it work. With formula being free and on the shelf at the food bank, however, they may grab it and feed that to the baby. Many of us know, when we start supplementing, we can quickly lose that breastfeeding relationship. The food bank may continue to have formula or they may not and we end up in situation like the above. How do we feed the baby in this situation? The staff at the food bank could use some education on breastfeeding and formula feeding. Many of them may still hold the belief that mothers with a low-quality diet shouldn't breastfeed, that it isn’t good for them or their baby. When formula is available, they may encourage that to a mother who’s breastfeeding because of this belief. Don't get me wrong here; the issue isn’t the people donating the formula to the food bank. They have good intentions and likely don’t realize the damage that can be done. The issue here is that this is exactly one of the things the formula companies want to happen. They want their products in the hands of the vulnerable new mother and father. This is why they send packages out, and they do it in the manner of “Breastfeeding is best; however when the time comes, introduce formula”. If the time comes to introduce it and continue with it, you will buy the kind that was free and came with coupons and other swag items like a backpack or change mat. It’s all marketing. How free do you think all that stuff was to produce and mail out? Not free at all; in fact, it’s in the high price of the formula. Let’s look at what formula is and why it costs so much. Those sending it out are a business and they need to make a profit. After all the free packages they give away, they need to increase the cost of formula drastically to make a profit. They’re so profitable, in fact, that not only are they giving parents free stuff, they buy the names and contact info of parents from the likes of maternity stores and giving all kinds of free stuff to hospitals and doctors’ offices. When a family legitimately needs formula, it’s so drastically overpriced that it creates hardships for them. What do I suggest we do with the free samples? I suggest they be returned to the stores where they came from with a note explaining why it’s being returned. Imagine if just a small percentage of moms did this. Would the stores start to think twice about their partnerships if they had a large number of packages to deal with? Another option is return to sender. I don't think this would have near the impact as the above option, but it would show them that you don’t want their products. As far as the moms who need the additional supports and are at higher risk of needing to use formula, there’s a better way to help those mothers feed their babies safely and reliably. This should go without saying, but the need to say it is always there. This isn’t about formula vs breast milk, nor about a mother’s choice to breastfeed or not. This is about an infant’s right to quality nutrition and food security, one of the basic hierarchical needs of the human race and a primary building block of children's futures. Breastfeeding can almost always guarantee an infant and child can be sustained.  Pumpkin patch I stumbled upon in Niagara Falls, 2015. Pumpkin patch I stumbled upon in Niagara Falls, 2015. Thanksgiving has me reflecting on my work as a doula & birth in general. I have to start with first of all giving thanks to my family, especially my husband, as the primary supporter of my work. Birth workers are said to have one of the highest rates of burnout. There are lots of reasons as to why (and I will get into that in another blog post). One of the reasons is that it can be incredibly hard to find work-life balance in this field. Without the loving support & patience of our partners, most of us would burnout and fail in this profession. If you have been lucky enough to have a doula by your side for your birth, know that someone else was likely behind the scenes, keeping the wheels moving on the doulas other commitments at home, and possibly even other work. It can take a village to have a baby, even though you don't want the whole village at your birth. Join me in a collective “thank you” to the partners of our communities doulas. I am thankful for mine. This Thanksgiving my extended family decided to try something new. Normally, we would gather at one of the siblings home and be graced with much food of the homemade variety. Our families dynamics have changes over the years and with that we have made changes to how we celebrate - natural progression in a way, but we have always kept a homemade, in home gathering as a part of it all. This year we did something much different. We were going to go out for lunch, 13 of us, Chinese buffet. Fabulous idea, right? No clean up before, no meal prep, no clean up after. We can leave all that work to someone else. We begin to arrive at the restaurant, one or 2 family members, or 6, at a time, only to discover, there is no lunch buffet. Some become disappointed because they wanted Chinese food, some are disappointed because it means loading the car back up and going somewhere else, some are becoming annoyed because finding new place for 13 people isn't all that easy, some are relaxed and happy to go along for the ride. We continue with the plan and head over to a family restaurant known to have a great buffet. We get seated at a huge table, spread out our family (for the record, my immediate family is half of the whole family, as visually seen as my kids and husband, sat in chairs on the outside, while my siblings and their family filled in the other side). We are eat and enjoy the food and company. All is well, this is a success. As we head home, I am feeling unsatisfied. I am physically full, but can feel an emotional void. It just isn't the same as other gatherings. Now what? I can't just leave this feeling. My approach is to plan a meal for my immediate family for the next day (which is now today). It shouldn't come to any surprise that I like tradition & rituals. That is exactly what was missing yesterday. That is what was leaving the void. Interestingly, traditions and rituals are what I enjoy most about birth work. There are “things” that just work. Today I meet with an expecting mother to discuss being a doula at her upcoming birth and one of the terms that came up was “wise woman”. “A wise woman is considered to be knowledgeable in matters such…traditional lore.” There it is, tradition, again. There are rituals that just work and that is what makes the difference emotionally. For me to feel satisfied in the holidays, I need to have that ritual of the work of prepping the home and the meal with expected dishes that taste as good as they feel good for the heart. Just like labour is work, it is a ritual that serves us emotionally as we prepare to give birth and become parents. We have lost birth in our community as changes have occurred, just like the changes that have occurred in my family over the years. My lesson this weekend is that getting back to rituals and understanding of the holidays and what truly leaves us fulfilled still needs to be there, as we work with changing family dynamics. Just grabbing any meal in any place served us as far as being feed, but left us emotionally empty. If you are expecting, grab yourself a doula, or someone who understands traditions and rituals in birth. They will protect that emotional space of having a baby because that is just as important as a healthy mom and healthy baby. This is a question the Pasqua South Medical Centre office staff often get asked when they make the recommendation to book an appointment with me. I am going to try and answer that question for you, and them. The centre staff may actually not know all the benefits of seeing me either. I am "new" to their space, they are getting used to me and gathering experience. They can see the improvements mom and babies are having, but they really do not know much about my services vs the free services. I bet it is safe to say that most people don't know the differences.
I am going to highlight a few. If you think of others that could be added, by all means leave a comment and I will add them in! 1) We, the client and myself, have a mutually agreed upon, prescheduled time. Free clinics often have you come in, take a number & sit and wait for your turn. They won’t likely know how many moms are going to show up, meaning mothers & babies (maybe fathers and other children,, too) could wait for quite some time and then be feeling rushed. They see all the other moms & babies waiting for their turns. At the centre we have a scheduled time, hopefully to your convenience and we allow enough time to avoid feeling rushed. Home visits provide a scheduled time AND the privacy and convenience of your own home. 2) I simply have more availability and flexibility. Not only is the timing better but you get more options as to when. Again, free clinics might only happen once a week. What happens if your struggles start on the evening the free clinic was being held and you missed it? Or sometimes you may benefit from two appointments only 2 or 3 days apart. A week can seem like an eternity when you are struggling. 3) I am an Internationally Board Certified Lactation Consultant (IBCLC). Not all the staff at the free clinics may be an IBCLC. The free clinics are staffed by Public Health Nurses (PHN's). Some PHN’s are IBCLC’s but not all are. I am an IBCLC dedicated solely to breastfeeding, with 10 years of experience helping moms and babies, 5 years as an IBCLC. (By the way, if you use the free clinic, don't hesitate to ask if the person helping you is an IBCLC. If you really wanted to, you could consult the IBCLC directory.) 4) Education is a high priority to me. I mean MY education and I mean YOUR education. I have attended, and continue to attend, a wide variety of additional & extended trainings and conferences. I have a strong ethical background to practice evidence based lactation “science”. I also want to give you enough information about what is going on with you and will answer all the questions you have. We book enough time to be able to do this. 5) In all my years of experience I have had access to ranges of breastfeeding from normal to extreme difficulties. My initial exposure to breastfeeding help was a peer-to-peer support group where our scope of practice was to help mothers by providing emotional support & information within “normal” breastfeeding. I got to know normal really well and be introduced to some not so "normal". I was super curious about those not-so-normal cases and pursued my IBCLC. Now I have much more training with the outliers of normal. I am also able to follow my own client cases much more closely to monitor outcomes and refine the plans along the way. This gives me the advantage to know whether the information and care plans I am sharing with clients really work. Often in a free/public setting you will be exposed to different staff member every visit and they do not have that same luxury. They might tell all the moms to do the same “thing” thinking it is best practice and not realize that is not useful for moms to do and they are not getting the desired outcome. 6) I have direct access to centre physicians if something is outside my scope of practice or comfort zone and we want or need a physician involved on some level. This is especially useful for further diagnostic testing or prescriptions we might want to consider. We have developed some great protocols together and collaboration like this is unique, yet so beneficial and much more efficient for resolutions of concerns. 7) It is my standard practice to do a through history of mother and baby. We need to make sure that we have all aspects and contributing factors considered when we are determining why there might be struggles. There are more factors to lactation than most people are aware of. I go much further beyond getting a better latch and a better position. We make sure to look at the situation from a few lenses. We pull out the puzzle pieces that might be problematic and piece by piece get the whole puzzle fitting together into a nice picture. You should hopefully be able to see what we are offering is completely different from what is being offered for free. You can count on focused, one-on-one care with a plan to approach the issues that brought you to me. You have the opportunity for follow up with the same person you saw originally and someone that can dialogue or report back to your physician and other care providers. I can help you address the specific concerns you have and reassure you what is the normal course of breastfeeding and give you my expertise with the more challenging aspects, with references and resources from the latest research. I can also make referrals and recommendations easily to a variety of other health care practitioners who may be of value to your specific concerns. I look forward to seeing all of you and your darling little ones. Please feel free to book an appointment at your convenience. Canadian parents need some awareness about the health and future health of their children.
It is said about 98% of mothers “initiate” breastfeeding after birth, in home and in hospital. At six months about 26% are still breastfeeding. Stats can be seen here. One of the primary reasons women quit is perceived low milk supply. We are all familiar with the arguments of “But, some moms just don’t make enough”, “I will try to breastfeed but if I am one of those mothers that cannot produce than I guess I cannot breastfeed”. Correct, some moms do not produce milk, but certainly not 75% of women. When worded that way, hopefully more people say, “yes, that can’t be possible”. Many women do have low supply. Low supply does not equal no supply. Low supply does not equal not having any ability to make milk. Low supply can very often be avoided, turned into full supply, or can be worked with in addition to supplementation. Low supply does not need to end all breastfeeding. What is going on then? That is not an easy answer and cases are all unique and need to be assessed however, there can be underlying answers that are similar or related. Some examples (the list could be much bigger) · Birth experience (trauma, separation, medications) · Supports (hospital staff, family, friends) or lack there of · Education (parents, grandparents, doctors, nurses, midwives) again, or lack there of · Returning back to school or work We seem to be setting the aim for optimal starts for our babies and children but we are not often striving to reach them. If we become derailed why are we not getting back on track? Luckily, we can get back on track when we find ourselves off track. You need to know this. We need to get serious about giving our babies the best start. Old arguments do not hold much weight anymore. “I was formula feed and I am ok (fine, survived)”. What is ok? What is fine? What is survived? We have overcrowded health care systems. And we have normalized this situtaion. Surprising to some, breastfeeding, or lack thereof, can be linked back to the majority of the health conditions that patients have. We need to normalize breastfeeding to reduce the strain on our health and wellbeing. We cannot rely on the system of disease care to be the system that is going to help support our babies getting off on the right foot – being exclusively breastfeed for the first 6 months and continuing to 2 years or beyond as suggested to be optimal buy the authorities of children health. (AAP, CPA, UNICEF/WHO) It is time to take charge of our own bodies and our children’s future. It is up to us to give our kids the best start that only we can give them. We need to move past the idea that we have free health care. We simply do not have free health care. We have access to (some) free disease care. Healthcare should be disease and illness prevention. This certainly is not free. We need to start being accountable for our own healthcare. This lack of accountability is why we have maxed out healthcare facilities and resources. If we had more accountability we would make better choices. If the system wasn't so strained right now we could suggest that we start to put disease and illness prevention first, but right now that isn't a priority of the system, even though it is the priority of many citizens. With that awareness we need to start at the very beginning of an infant’s life and choose breastfeeding as a key to lifelong health. There are lots of old arguments. It is time to let go of those. This is not about past choices, which were based on “what we knew then”. We know more/better now and when we know better we do better.  What do we really know about breastfeeding? Really? We are 3 generations into formula feeding. It’s been said it takes 100 years to make change and make things the norm. Well, indeed, this has worked for formula feeding. That is by far the most common method of feeding infants DESPITE a whopping 90+% initiation rate in our country. We are failing more than we are succeeding which tells me we don't really get it. Why are we so quick to start supplementing or letting go of breastfeeding? What steps are we walking before we made that decision, if any? We should be working to remedy breastfeeding but this idea that we can supplement while we remedy breastfeeding, isn't a wise one. I am not saying supplements are not needed at times but I am saying that our helpers should know how to work with breastfeeding first and foremost. Why are only a quarter of babies getting any breastmilk by the middle of their first year? A very large part of it is that there is a fabulous amount of interference. Interference comes from all over and starts long before babies are even born. Dare I say this interference starts before most babies are even conceived? Let’s look at media. Let’s look at the propaganda all over medical establishments, directed both at patients and at medical professionals. Let’s look at our own communities and then our own families. What is the message out there reaching people? Could this be part of why we are not able to help remedy breastfeeding? They are certainly not breastfeeding friendly messages. But, let’s say you get through all of that and to the people that are supposed to be promoting and supporting breastfeeding. You know what? You still will here a large amount of variants in what these people say and recommend you do. From basics of position and latch to troubleshooting concerns, it seems very few of us on are the same page. It is highly frustrating as a professional and I know it is highly frustrating as a parent. It honestly makes me ask myself, what do we know about breastfeeding? For many years I was involved with a peer support group. Within this group I was told that this is where we see normal breastfeeding. It was a well-established group with many, many years of experience in breastfeeding. This was my introduction to breastfeeding outside my own experience and being able to view and witness many dyads and what breastfeeding looked like for others. It was amazing and eye-opening. I learnt lots and went on to learn more and become a peer-volunteer to help mothers that were struggling. I was all in. Consuming all I could to try and figure out the barriers to successful breast-feeding. I had a big blue book full of breastfeeding information. I studied it. I did activities and exercises to help me expand topics. I read and read and discussed breastfeeding at great length. I was accredited and able to start helping moms. Moms would call me with concerns and I would look up moms concerns and then read to them from the book what the strategies were to help them overcome their challenges. I very often never heard back from these mothers to know if things resolved or not. I am hopeful many mothers did better and were successful but I know now that lots did not. I saw many moms in person return to meetings month after month and got to know many of these dyads well. We told mothers what they could do right to make breastfeeding work well and especially how if people didn’t interfere all would be good for them. Feed early and often and supply would be there. Don't have pain meds in labour and baby will breastfeed well. Stay away from bottles & supplements and pacifiers and just feed and feed and feed. Yet, that didn’t work for everyone. I really was perplexed as to why. After a few years of this, that is when I decided to expand my education and knowledge and scope of practice. I was going to pursue being an IBCLC. I mean, I knew normal breastfeeding, right? How hard could it be? Was becoming an IBCLC easy? Not at all. Was it hard? Yes, indeed. On so many levels. I was shocked when I started getting assignments back with really low grades. So many wrong answers. But how? I KNOW breastfeeding. I have been helping moms for years. I have these answers in a big blue book. It says here in black and white this is how breastfeeding works and this is what you do to overcome the struggles. It was wrong? How could it be wrong? How many women did I tell this info to? And how many of my friends did what the book said. This is how breastfeeding is, this is the normal for breastfeeding and all moms and babies are different and that’s ok. But I came to learn, yes, some concerns are common but there are actually tighter perimeters on what is “normal” and expected. I was pointed in a new direction for learning. My beliefs shifted in a few ares. Change is hard. But I was changed. I started seeing stuff in different ways, through many different eyes, many different versions and was taking a critical look at what I knew and what I was learning and the work of many others. I learnt about growth charts and poop (oh how I love to talk poop now), infant sleep, tummy time, newborn weight gain and loss, milk supply, medications, medical conditions, how to supplement and when it actually is helpful, and how much happier and less stressed some moms and babies (and their families) could be and how to screen the bigger picture. I learnt more than how to tell moms more than “this too shall pass” & “some babies are just like that”. I also learnt that professionals don't agree on a large number of topics. Weight loss, sleep, pain, creams, positioning. When and why did someone decide that 7% loss if ok, but 10% means we must supplement? Why do some think there should be zero weight loss at birth and some think it is acceptable to take 2 or 3 weeks to get back to birth weight? Why do big babies need to be supplemented an hour after birth but small babies are ok? Why do some say that sore nipples is a right of passage and some think there should be no pain, ever? Why are some nursing babies like footballs and other think we rarely should do this? This list could go on and on. For some of use we come to our own conclusions based on clinical experience and patterns and outcomes that we see. Some of us just read the guidelines laid out for us because that is how it has always been done. Some of us are halfway between. Some of us come from a place of our own experiences and judgement and biases that come from that. (The latter is really not best practice and we need to learn how to detach from our own experiences to look at the current evidence in front of us.) Some of started in one place and have landed in another. I can say that I believe I do have good evidence based research to back my opinions on many of those questions, plus many others. I have protocols and practices that I use over and over with success with families, but am happy to say as much as they are protocols they are very flexible and can be defined differently for each family. I haven't stopped seeing stuff in different ways, through many different eyes, many different versions and haven't stopped taking a critical look what is happening with my clients and figuring out how I can best help them met their goals. Ladies (& partners and support people), you need to know that there are resources out there to help you, when you need it, where you need it and that will consider YOUR goals. I can come to your home, I can come to see you at the hospital, you can come to my office. If you feel like you are not getting the support you need, when you need it, don't throw in the towel on breastfeeding. There are always options. Breastfeeding can take some time to get established. It is a learned behaviour by both mother and baby, and each baby a woman has is a new learning experience. With that said, time is also precious when trying to get breastfeeding established. Some things are normal learning curve experiences and some things are not normal and should be addressed as soon as possible. Mother's almost always know when something is not correct. I spoke with a mother earlier this week who knew something wasn't right. She asked for a referral to a lactation consultant and was denied. She continued to ask as the days went on and was told repeatedly that what she was experiencing was normal and wasn't yet at the point of needing a lactation consultant. Her frustration was to the point that she was ready to throw in the towel on breastfeeding. She spoke to a friend who informed her that there are private IBCLC's who she could see and who would be able to see her sooner than later and that before she quit breastfeeding she should call me. This mother took the advice of the friend and gave me a call. I was able to listen to her breastfeeding story to date, do an assessment on her and baby, figure out what her goals for breastfeeding were and prioritize the concerns she had about breastfeeding. Sometimes it is about addressing one big issue, like the amount of pain a mother is having, and then moving forward with other plans and goals. Breaking it down into manageable bits and pieces can make the big picture seem far less daunting. Let's not worry about breastfeeding until baby is one year, if we are not even sure we are going to make one week with the amount of pain we have. Maybe we should look at how to get rid of the pain, and see how week two goes…sounds far less scary than pain for a year.
Guest post by Rhonda Young-Pilon Tired of being tired? Look no further! We have a solution for you! Non-Sleep Training (not a registered trademark) is the LATEST solution to all that ails you. Step one of this innate process is to start considering even before you’ve started your path to parenting that your life may not be shrinkwrapped into a perfect and neat little package. You did it through the late years of high school and maybe even through college – studying into the night, slamming back coffee at 4am and cramming in three more hours of studying, writing the big exam, and then PARTYING because it’s done… followed by waking up in a tousled mess of blankets, books, and coffee cups and THEN going into work for the weekend and doing it again the next week. You made it. Even though, at your wedding or celebration of domestic partnership your grandmother whispered into your ear that having children would be this wonderful, golden, perfect start to your perfect white fence life and EVERYTHING hinged on routine, routine, routine. You thought you were set, right? Well, look no more – step one is ALL about breaking the rules of the grandparents and friends around you who are bragging about their perfect little bundle of joy who sleeps all day, all night, and even allows for time to Kon Marie your entire life! What’s the evil baby meme say? “You will never sleep again”. It’s partially correct. Step two of this process is to, of course, design your cave. Kon Marie is partially right – you need to get rid of things. Or, in our program, you need to find a place to put things until you can slowly release them back into your home once your screaming bundle has become a compliant pre-schooler (ha). Your cave needs to have darkening capabilities. Maybe two o’clock in the afternoon is when you will catch a nap – just like you did after the long exam, during the bad hangover, or when you’ve had a tough week at work. Does the laundry pile matter? Not necessarily. It’s merely one of the many tasks that you can assign the adoring baby-doting family who comes over. Letting them see your postpartum stained undies is optional with our system, of course. Other assigned duties may include – vacuuming or floor maintenance, walking your dog, dropping by meals, or even partnering with another family to do some weekly trade-off of cooking. The cave, in itself, needs to be designed as such that sleep can occur at any time, and that entertainment exists when there is a need for the other partner to rest for work purposes. Maybe your cave has a jar full of ear plugs and a written agreement that each parent shall split the sleep into shifts. Entirely up to you. Fred Flinstone-style beds are optional (if you recall, sometimes they slept together and sometimes they did not).
Are you NOTICING that none of these sleep regiments involves the baby? That’s step three. If the caregiver is set up to be able to function around the baby, to keep the anxiety related to not having perfection, then this tiny little bundle of joy will get there. Humans tend to enjoy darkness for sleep, but it’s a process that takes time, patience, and definitely not $10,000 and a personal consultant to dole out advice that is essentially well known to be true. The strategy is to not buy stuff or professional services – but maybe looking to gain support if that’s what you feel you are lacking. Maybe you could be spending your money on professional services like a IBCLC to come in and help establish breastfeeding so that isn’t another factor, or a loving house keeper to come in once per week and help you to tackle the laundry pile. Maybe that money could be put into trust for your little night owl’s college education, because, let’s face it, someone needs to stay up all night and catch babies, engineer products, and write the next big hit. Step four would involve strategic sleeping, enjoyment, and something called pillow therapy. Some people recognize the term “pillow therapy” as a method of smothering… however, in this case, it references when you go into your bedroom and shout insults into your pillow. Sometimes, you need to escape your emotions somewhere that isn’t the face of your partner, or in the face of your baby. It’s been two days since you’ve slept more than a two hour stretch, your partner has been away for days on a man-cation/woman-cation, and you desperately need to shave your legs… it’s time for a release of that emotion. Beware, it may cause tears, a desperate call to a friend to come by for a few hours so that you can nap, and a strategically scheduled glass of wine later in the evening. It all comes back to support. Single mothers – I hear you. This sleep solution involves recruiting a well trusted friend who loves babies to snuggle while you snore. There are many local church groups who may have a wonderful grandmother who just happens to have recently retired and is missing out on baby cuddles due to empty-nest syndrome… there may just be someone, in your community, who can fulfill the position that you need for temporary solutions. Moms often ask if napping is required in order to establish routine. Certainly, in utero, your baby could be lulled to sleep with gentle swaying, darkness, or following a long day of movement. As soon as you reach the fullest complement of pregnancy, your skin stretched to its height of stretchiness and your baby was able to have it’s first exposure to light. This is what initiates the pattern of knowing that change existed. Of course, our wish is that our baby will have one to two excellent naps through the day, have a period of play and wakefulness in the evening (and contentment, which is basically a ruse historically), and then a long period of sleep through the night. Babies are wired to require things like closeness, suckling at the breast, quiet, and little stimulation in order to accomplish these things. Hence the design of your cave. If the cave presents itself for opportunity, you’ll probably get there. Of course our caves aren’t designed with boobies strategically placed next to the crib or computerized baby swing – so we are bound to be attached to our infant to provide these needs. There are several baby carriers on the market which can allow moms to enjoy hands free, baby to enjoy the boob and nap, and for all to get to those important places that we are required to be during those first months of life. Maybe your $10,000 fee for a consultant could go towards purchase of the best lazy-boy recliner on the market and a well-stocked side table? Step five includes the warranty. Manufacturer’s guarantee, that humans can survive on strategic sleeping (grown up humans, that is). This may extend well beyond the first year of life, and into toddler and preschool and school age years. Children have complicated wiring that comes to life – and some of our kids sleep less than others. You’ll start to load up your arsenal as life goes by – with tips and tricks like the evening walk, the warm bath before bed, the “fill’er up” healthy bedtime snack, and even the occasional night at grandma’s house. It comes with time and patience, and knowing and trusting that a normal infancy may create a new life for you. Many humans before you had to leave the cave at some point to tackle a tiger, collect water, and to visit friends. It’s all part of essential survival. Step six of our survival kit includes some optional equipment. Many parents have employed the tools of distraction – these may include things like make up tricks, hats and scarves to cover up mis-placed hairs, coffee makers and even coffee to go into the machine, and the best sweat pants on the market. These days, messy hair is in. Men have pointed out that women in yoga pants may be more appealing anyway. Dads may also feel the need to sport a sleek black Ergo baby carrier while their wives crack open the tool kit. It is well known that there will be a community of people who, like them before, also sported the exhausted looks and will usually signal their commiseration if they are privy to the reason for the bags under your eyes. Sometimes, your husband/partner will come home from work and tell you that their dazzling co-cubicle partner also struggled with the sleepless nights. Who knew that the tools and tricks of the trade meant that the “perfect” parent seated next to you survived by guzzling two litres of coffee and crying in the car on the way to work! The idea of this essay is to normalize what parents believe should be categorized as abnormal. In my opinion, as a parent of three sleep-disabling children, this world is too focused on perfection. It’s also an example of what we are expected to be, which isn’t fair to this earth. I do not see it a fair trade to pay a consultant thousands upon thousands of dollars in return for kids and parents who don’t ever experience hardship. The secrets to raising kids who are well rested shouldn’t cost money, and should not result in parents having to stop comforting their babies, or to sacrifice breastfeeding in order to survive. The idea is that we all work together to bust down the brick walls of our homes to support each other through those terrible days. If mothers opened their doors and yards to supporting their neighbours, then we would see a better rested society. Traditionally, in a tribe mentality, grandmothers, aunts, and other women would support a new family so that everyone got what they needed. We don’t live in a tribal society, and therefore we need to seek out the same sources of support. The real trick of the trade is to seek out rest and support where needed. The early days really are hard, and mothers need to know that they are at an increased risk of postpartum mental health crisis when support is not given. It doesn’t mean that mother in law needs to move in – but, for you, it may mean that mother in law needs to stay in a hotel near by and deal with the rest of the house so that you can stay in bed with your baby and enjoy life. Maybe it means that your husband needs to dedicate his evenings to honing his skills at cooking and that weekends are when the house gets worked on. It may mean that a friend may step in as a caregiver for your other children so that you can be skin to skin with your baby. The long lagging months and years with little bits of sleep do affect us cognitively, however, with some peace and relaxation – we can all be on the hammock in the warm back yard having an afternoon nap. Nobody wants to “sleep when baby sleeps” when there is chaos. It’s ridiculous to expect us to never leave our houses or experience social time because the regiment will be thrown off. We need to find the balance, and as a community support new parents in their journey. That’s worth $10.000/parent. In the area of breastfeeding support, education and advocacy often times those of us in this line of work are assumed to be anti-formula and not willing or unable to support the formula feeding families. People are often shocked to find out this is not actually the case, or at least not always the case. More and more within the education and work I do, we are discussing the non-breastfed baby. As we learn more about breastfeeding, we learn more about babies, mothers and families and the needs of babies, mothers and families. One of the most recent headlines that started a discussion between myself and a couple of friends was that breastfeeding has a positive effect on the mental health of children and adolescents; in fact the longer the child is breastfeed the more significant the benefits are. Interestingly, in this information released was the need to look at how the non-breastfed baby can be given similar benefits.  To do this we need to ask, what is it about breastfeeding that makes for this benefit? Is it the “milk” factor? We know that the fatty acids and other non-replicable components in breastmilk are great for brain development and growth and those hormones like leptin protects against stress in infants. What about the attachment factor? We know that breastfeeding mothers look into their baby’s eyes more, they touch their baby’s more, there is more skin-to-skin contact and in fact breastfeed babies have a stronger relationship with their mothers than with anyone else. Breastfeeding is a relationship builder between an infant and its mother. It is the first secure, attached relationship that a baby learns to trust. Healthy secure, attached relationships have been shown to be have a positive effect into adulthood. Are there other factors to explore yet? We can see that it is potentially a combination of factors that lead to this finding and benefit. Exploring the factors, I am able to answer the questions that arise from the mothers that are not breastfeeding when they see a headline like “Breastfed babies have fewer behavioural problems”. They do have honest questions of “What about my baby? Breastfeeding did not work for us.” (we do not need to get into the why it did not work here, that is a whole other blog post, or 10). They ask to be supported as equally as a breastfeeding mother would be or sometimes they do not ask for support at all because they fear the reaction. They might expect to see an eyeroll when they say they need to be supported as well. They may be unsure of what reactions they will get. They may expect to hear someone say if you would have tried harder you could have breastfeed or hear the stat of how many mothers truly physically cannot breastfeed. So well this *might* be true, it is sometimes too late for that information. Giving that info for future babies or other people they might support later can help, yes, indeed it may, but it does not answer the questions that she is asking right now; the question of what about my infant that I am not breastfeeding right now. I want to reassure these mothers that it should not be an eye roll and they deserve the information and support they need at that time. To these mothers, I say, goodness, if *I*, the one who will not say that formula feeding and breastfeeding are equal or that we should not continue the work we are doing for breastfeeding globally to have higher rates, longer durations, etc, can say that we still need to educate and support these mothers on infant feeding then more people should be able to see that. Like I mentioned, it may not be all about milk. Certainly, when you place breastmilk beside formula there are vast differences, that science cannot be disputed and formula companies will never come close to replicating breastmilk. Does that mean I would be happy if all babies had breastmilk from a bottle and were never at the breast, never held for feeds, never caressed by its mother? Certainly not. We need to educate society about the ACT of feeding infants and caring for our infants and the impact of these actions, good and bad. A question that serves food for thought that looks at just this idea; "If you had to choose one of these options, which one would you choose? 1) Would you breastfeed with formula being the substance that came out of your breasts or 2) Bottle feed breastmilk?" More questions arise around the impact of pumping breastmilk and bottle feeding vs feeding directly from the breast. Every mother will answer these questions in their own unique fashion, based on their experiences, education, situations and perceptions. Existing are the ideal, perfect breastfeeding relationships and co-existing are the handfuls of many "good enough’s". Good enough is not necessarily a bad thing. It can be a place of peace and harmony for those mother-baby dyad’s. Do I strive for 100% of the parents I help to have the best, most wonderful breastfeeding relationships, or can it be "good enough"? It would be so wonderful and we would all be fortunate to get to 100% but is that realistic? For now, good enough is acceptable for me when it is the choice the parents. We get there when parents have been supported and educated in the decision making process, as all parents should be. It might mean breastfeeding solely, artificial feeding or mixed feedings, it might be direct breastfeeding, it might mean pumping and bottle-feeding. Every families good enough will always look different. Where we fall short, I feel is in completing this responsibility of educating and then supporting, period. This is where I think “good enough” is not acceptable. This is where we need to improve and this is where I plan to focus. If you need support & education I offer a variety of services - doula support, lactation support and prenatal birth & breast-feeding classes. Contact me to find out more  Disclaimer: I am not a mental health care professional or provider. If you think you are suffering from any sort of mental illness I recommend seeking medical attention as needed. I will also add in that I do take mental health concerns seriously and this blog post in not intended to down play medical concerns. Before you diagnose yourself with depression or low self-esteem, first make sure that you are not, in fact, just surrounded by assholes. - William Gibson When I first came across this quote, I immediately identified to it as an adult, as an individual and as I related to other adults. More and more I have been thinking about this in the context of my work, my work with new families, young babies and children & different relationships forming in homes. The rate of postpartum mood disorders is on the rise. Baby blues, anxiety, depression and psychosis are a very real reality for many new mothers and fathers. We mostly see it in the context of mothers but more and more research shows our fathers are impacted by mood disorders as well. Let’s, however, just step back for a minute and think about the above quote. “Before you diagnose yourself with depression or low self-esteem, first make sure that you are not, in fact, just surrounded by assholes.” I don’t want to be rude but let’s face it, babies are assholes, toddlers are assholes and kids can remain like that as they grow up. They certainly don't mean to be but they are incompetent & demanding, they can be obnoxious and rude, they interrupt your every meal and all your sleep. You can’t even think about peeing without baby waking up and crying, let along move an inch to try to get up and pee. They need to be fed constantly, hanging off your breast, YOUR breast no longer belongs to you. When they are not feeding, they need you to hold them or they will turn the reddest of red and blow horrible smoke from their ears. They pee and poop ALL.THE.TIME. Rudely, they sometimes don't even wait for the new diaper to get on before they shit all over you or shower you in pee. You imagine stuffing that thing back inside you, because as awful as it was to have that watermelon come out the lemon, they are way easier to take care on the inside, right? Well, too bad, there is no turning back. There is only moving forward with this asshole in your life. By now you know I am not serious in calling babies assholes, but you can see my point. Life is HARD with a new little person to care for. The real assholes of the world are hard enough to put up with, but now you have to put up with the smallest of them all, ALL the time, because YOU created it after all, YOU wanted this. Now you have to do it when you have zero sleep, zero nutrition and probably zero clue how to actually take care of this baby - I can guarantee you it did not come with a manual. Add in some hormones and everyone’s opinion of what you should be doing and it is easy to see why one would end up with signs and symptoms of a mood disorder or postpartum depression. So, how about we get serious about what we can do about this baby and get through what will be one of the most challenging times of your life. Self-care is big. You don't want to lose yourself in this. Having a baby WILL change you, but doesn’t need to consume you. What do YOU need? What does your partner need? Make a plan to have that happen. 15 minutes in the shower, making two sandwiches instead of one when your partner leaves for work, tea out with friends. Asking friends to bring you food when they come visit the baby. By the way, when they come visit, the asshole will switch personalities and put his nice guy face on. Have someone come help with light house work and laundry once a week. It’s the small things that make a massive impact. Communication is huge. Tell each other how you are feeling about the changes in life and the new demands. If you are reading this before having your baby, start that conversation now. Brainstorm the different ways to achieve self-care that will work after baby. Be open and flexible in changing those plans, if needed. Just talk to each other and others about what is happening in your new world. Just keep the conversations going. And find others who will listen to you both. Just someone who will let you get it out. I promise, they won't mind. Support. SUPPORT. SUPPORT. This is a must. You need to build a team of support people. Before baby is ideal but may not have happened and you may now just be building a support team. Who are we talking about? Family, friends, community resources - your health care providers, doula’s, peer support groups. Everyone’s team is going to look different depending on the needs they have. What is important to know is that support is going to make one of the largest impacts in how you feel about everything and how stable your mood will be, how you will interpret your experiences and what the outcome of the situation is. It is important to identify your needs and equip yourself with the tools to get there. It is vital to know what your support options are because without options you have no choices. So, start now by identifying your needs and making a list of supports. If you get lost and have a need but don't know how to get the support you need to have that need met, please ask! I am here to help in this time of transition in your life.  In 1988, over 25 years ago, the Supreme Court of Canada ruled that discrimination against pregnant women is a form of discrimination on the basis of sex. The biological fact is simple; only women have the capacity to become pregnant and therefore discrimination on the basis of pregnancy is a form of sexual discrimination. In Saskatchewan, as in other provinces in Canada, women cannot be discriminated against on the basis of pregnancy. This is upheld in both the prenatal and post-natal period. Women who are expecting or have recently given birth are entitled to reasonable accommodations that may be necessary because of their pregnancy or having a baby. In Saskatchewan, this included women who are breastfeeding as stated by the Saskatchewan Human Rights Commission. One is left to ask them, why is it that after 25 years since this Court ruling, are breastfeeding women still being discriminated against? Experiences of Saskatchewan women being discriminated against in the last two years include mothers being asked to stop breastfeeding on public transit, a lifeguard at a public pool asking a nursing mother if she can go to the change room to nurse, in another pool in another city a mother was asked to get another towel to cover, another mom is asked to stop breastfeeding her infant while she is in a family restaurant and a mother was kicked out of a mall for nursing in the food court. The list has more, that was just a few. I am left to assume that the people who complained about these women and the people who asked them to stop nursing in public did not think of their actions as being discriminatory and least of all against women on the basis of their sex, but it is. We need more public awareness because these occurrences create barriers for all mothers and their babies. Furthermore, staff and establishments could be left paying a legal consequence because patrons have asked staff to intervene. Who gets to tell the patrons that they are indeed wrong and that the staff cannot and will not approach the mother and child? What if the staff does not know and they approach the mother and child? Legal consequences fall on whom then? The public needs to be aware of this law and the rights of the mother baby dyads as do businesses and their staff. It would seem as if society is behind the law on this act, this biological act and need of all infants. It is time that society steps forward 25 years on this issue and catches up to the law. The evolution period of this law has had more than enough time. The laws can help shape societal norms and I, for one, think that it is time this law comes into play to help move the norm of infants and children breastfeeding in our society. It is no longer socially acceptable to drink and drive and the laws definitely helped to raise people's awareness of the serious consequences of that behaviour. The laws that protect people against discrimination on the basis of sex have been around for many decades in Canada. These laws are included in the Canadian Charter of Rights and Freedoms, which is part of the Constitution - the highest law in our country. The fact is that women are still being asked to cover-up, move or leave venues, almost 25 years after the Supreme Court of Canada’s decision that discrimination around pregnancy and childbirth and breastfeeding is discrimination on the basis of sex. Societal norms in regards to breastfeeding have not changed to keep up with the law and it is time that it does.  Pain. Ouch! Why do we get pain? Pain is your bodies way of getting your attention. It is a system in place in our bodies to protect itself. It is a “red flag” or “warning sign”. It is telling you something is happening that you need to pay attention to. Sometimes it is telling you to pay attention before you cause an injury. Sometimes it is telling you to stop what you are doing, sometimes it is telling you to do something else, sometimes it is telling you to rest. Pain accelerates healing, because we will rest injuries; most of us need a reminder to rest until healed. So why am I talking about pain as a doula and as a lactation consultant? We can experience pain in labour and birth and with breastfeeding. The experiences differ, yet can over lap in areas. In labour we experience pain for various reasons; to tell our body to pay attention to this very important event, to tell ourselves to get somewhere safe, to tell us to rest. Our pain can diminish if we listen to it during childbirth. It can lessen with support, safe people, rest. It can really be heightened when we are scared, not supported, not in a place we are comfortable and exhausted. We cannot stop this pain by stopping the process. Labour and birth need to continue so we have to simply find ways to cope (medical and non-medical options as needed). There are lots of options available and a doula always has ideas in her head about how to get women more comfortable. Good childbirth education classes can also give a good understanding of birth, how it works and how to make a plan to minimize the pain. With breastfeeding there really is no degree of normal pain that we need to just work through. There is trauma, injury, infections, fear, stress, etc. Again, we need to figure out a way to cope. The body is saying “something is wrong, do something else” or “rest the breast” but, of course, that is easier said than done as babies nurse every couple hours around the clock for the first few days/weeks. This sort of pain needs to be addressed. Most causes of pain in breast-feeding is position and latch, so that is the starting point. If it continues, it is worth investigating further with skilled lactation help to stop the source of the pain, make a plan to heal from what is causing the pain, stop the source of the pain and get to comfortable breastfeeding. An IBCLC is a terrific resource for resolving these sorts of ongoing concerns. The idea of Doula’s are based upon old, old history. Old birthing history has so many stories of women with women, supporting and uplifting, during birth. In today’s birthing world many things have changed from the past. Change is good, but can also lead to having good things getting lost in translation. Having solid support for the body & mind throughout birth is one of the things that was getting lost, but in recent years more and more women are choosing to hire a doula.
“Doula” means “Woman servant" or “caregiving" and we adopted it from Ancient Greek language. “Doula” has now come to mean someone who provides emotional, physical and informational support. Doulas nurture a woman and her partner throughout the birthing process and afterwards. Doulas learn the desires and wishes of the expecting mother and partner and help them meet their goals. If the goals need to change a doula helps facilitate the unexpected changes. Doulas do not only attend home births - they attend all births. Doulas do not only attend water births - they attend to mothers wherever mother is comfortable. Doulas are still vital when a woman has a midwife - they are not the same, they are complimentary. Doulas do not replace the father or the support persons - they add an additional layer of support and help support the father and support persons. What can you expect from a doula? You can expect they will help you prepare and educate yourself for the birth. You can expect they support your wishes for the birth. You can expect them to be with you for the whole of the birth process from the time you need them. You can expect them to listen to you and be compassionate to your emotional vulnerability. You can expect they will hold a safe and protected space for you. You can expect no judgement. You can expect they will hold you up. You can expect they will take your lead. You can expect they will lead you when you don't know where you should be headed. You can expect them to make your physical comfort priority. You can expect them to make your emotional health priority. What you can expect your doula NOT to do: • Doulas cannot do medical exams, tasks, diagnose conditions or deliver babies. Doulas are NOT medical professionals. The evidence for doulas show* ▪ 50% reduction in cesarean rate ▪ 25% shorter labor ▪ 60% reduction in epidural requests ▪ 30% reduction in pain medication use ▪ 40% reduction in forceps delivery ▪ 40% reduction in oxytocin (pitocin) use *Stats from “Mothering the Mother” by and Marshall Klaus, John Kennell & Phyllis Klaus. Choosing a doula can seem to be a difficult task, but keep in mind there is a doula out there for everyone.  We have come to a place in Canada where the previous less than mainstream idea of Midwifery care has come to a place of greater acceptance and desire and more understanding that Midwifery care should be the mainstream care a pregnant woman receives. But the acceptance and desire of this kind of care has increased much faster than the profession can handle and in some areas faster than the systems that insure and employ Midwives can handle. This is a Canadian problem, some would even say a Canadian crisis. In Saskatchewan, we have what some people would consider significant growth and what others would consider not enough growth, in the very recent years. Legislation came to be in 2008 but we didn’t see Midwives practicing until 2010, I believe. Many of the Midwives that practices pre-legislation could no longer practice due to legislative changes. Midwifery was left in limbo for a few years. Since then we have had 13 midwives in 3 health regions be employed. If you do the math, that is a big increase, but when you start at zero, anything is an increase. If you look at the number of pregnant woman and babies being born, it isn't going down. Here in Regina, we saw two midwives providing care for RQHR in 2011 and in 2012-2014 that increased to 5 positions, with 4 of those positions typically filled at a time. Those three new positions have seen a few changes over the years as we have had Midwives come in and out of those positions. RQHR has recently let clients and the public know that soon Regina will soon to down to only two Midwives. Likely within a month of this blog post, two of the 4 midwives we have will have moved on from Regina. So, what does this mean for midwifery in Regina & care that woman, babies & families receive? In short, it means a lot, but it can also mean very little. Women in Regina have tried everything they could to secure midwifery care. From calling the program as soon as they got a positive pregnancy test, to calling weekly to see if they have changed from a waitlist to a “yes”, and pleading for a home birth - something only midwives can provide on certain limited conditions. The waiting list is already rather large, 30+ women a month, and most women still end up in physician care currently so a plan B is needed. The biggest factor affecting potential midwifery clients is going to be that home birth component - or rather the CHOICE of birth location. Midwives can do home or hospital births but only midwives can attend home births. Within RQHR, there must be two midwives available and present in order to have a planned home birth. The choice of birth place is a huge benefit to women and families and one that I understand tremendously. But I want people to know, that births in the hospital setting can be wonderful, sometimes equally so to a home birth. Part of it is in the mindset of the family. Some of it is care providers. Some of it is support staff & some of it is the support people that the family choose. What else midwifery care offers is typically more time to get to know your care provider; (typically) care starts earlier, appointments are longer and there is more dialogue about options for care - like testing and other procedures that are offered. But what many people don't know is, you can have that dialogue with the care providers you do have and you always have choices and always a right to informed consent. So, yes, midwifery care “follows” that logic in nature but other care providers will meet you at that place when engaged. If your care provider is not willing to do so, then perhaps a new care provider might be a better fit for you and your family. You do have that choice. I will have it be known that I have had clients equally as happy with midwifery care, as they were GP care, and OB care. Often it comes down to simply being heard & being respected. Any good provider is capable of that, regardless of their title. Having a midwife isn't a guarantee of that. Not one care provider or support person can guarantee any sort of birth experience. Another factor that really makes a difference in how people feel about their birth experiences is whether or not they felt supported along the way. What many people don't know is that this is exactly what doulas do and is the primary goal of doulas. To support the family - emotionally & physically and with information. Your doula, much like a midwife, would have longer appointments with you, they would get to know your desires and wishes and would help you make a plan to get your desires and wishes. They support you regardless of birth location & care provider, they support you regardless of change in plans, they support you during those changes, so that you can still feel good about them. They help you find your voice and find it again if you have lost it and need to make sure your wishes are respected. They work for you, and with you, to get you to your goals. At the end of it all, with physician care, and sometimes midwifery care, and the support staff, you do not know who is going to be attending your birth, and you may see different people come and go as the shifts change. With a doula you can count on at least one consistent person who knows you, is there for you, understands what you want and won’t leave your side. Care providers are very important in pregnancy and birth but it isn't something I think people should get too hung up on during the pregnancy and focus too much attention and energy into. I think that energy is better spent cherishing the pregnancy, making sure mom is staying healthy by good self care, that baby knows that s/he is loved and welcomed to the world, that good plans are being made for the birth and someone is there supporting and encouraging this experience and the family. In an ideal world we would all have the choice of care providers and who receives our babies into the world, but when we do not have that option, we cannot dwell on that loss, but should instead focus our attention and energies where we do have control. Getting a doula can allow all that goodness to happen and you always have control over who your doula is. |
Kim Smith
|

 RSS Feed
RSS Feed
